Back
Poster, Podium & Video Sessions
Podium
PD25: Health Services Research: Practice Patterns, Quality of Life and Shared Decision Making II
PD25-05: Changes in Health Behaviors among Low-Income Uninsured Men with Prostate Cancer
Saturday, May 14, 2022
10:10 AM – 10:20 AM
Location: Room 244
Allen E. D. Siapno*, Megha D. Tandel, Lorna Kwan, Mark S. Litwin, Los Angeles, CA

Allen Enrique Siapno
Medical Student
Charles R. Drew University/David Geffen School of Medicine, UCLA
Podium Presenter(s)
Introduction: Men with prostate cancer from low-income and uninsured backgrounds have poorer health outcomes partly due to higher risk of chronic disease and lower rates of healthy behaviors. We sought to describe the changes in health behaviors of men with prostate cancer participating in a disease-focused treatment program providing free medical care and navigation services.
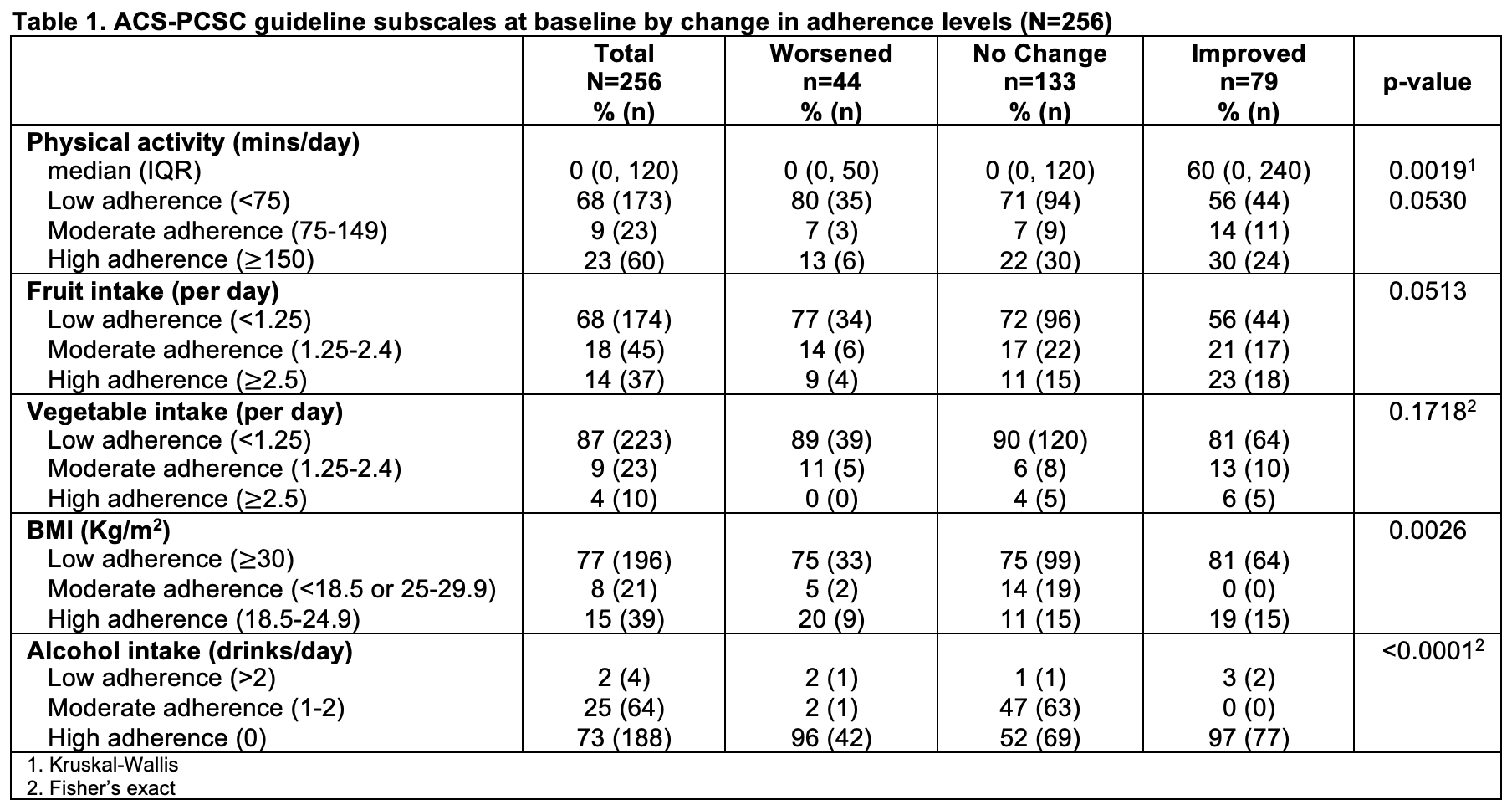
Methods: We retrospectively reviewed survey data from the UCLA Men’s Health Study, a cohort quantifying patient-reported outcomes, and compared baseline surveys collected at program enrollment to 12–18-month follow-up surveys. Five health behavior domains from the California Health Interview Survey were individually and compositely scored based on adherence to the 2014 American Cancer Society Prostate Cancer Survivorship Care (ACS-PCSC) Guidelines. The scores were categorized into three adherence levels: Low, Moderate, and High. Subjects were grouped by change in adherence levels from baseline to follow-up as Worsened, No Change, or Improved. We compared patient demographics, clinical characteristics, health-related quality of life, and adherence to the five domains at baseline between the three groups.
Results: Of the 256 subjects eligible for analysis, 17% worsened, 52% had no change, and 31% improved in overall adherence. Most subjects identified as Hispanic (72%), were foreign born (79%), and had a partner (71%). There were no differences in clinical characteristics among the three adherence change groups. Baseline general and physical health scores were similar, but baseline mental health scores were lower in the worsened group compared to the no change and improved groups (44.3 vs 50.1 vs 47.6, respectively, p=0.0320). Those in the worsened group already had low adherence to physical activity at baseline compared to the no change and improved groups (p=0.0019) (Table 1).
Conclusions: In this cohort of low-income men participating in a free navigation-based prostate cancer treatment program, 31% had improvement in overall adherence to the ACS-PCSC Guidelines for health behaviors. Worsening adherence was associated with lower baseline mental health score and physical activity adherence. Interventions aimed at physical activity may improve overall health behaviors.
Source of Funding: Department of Urology, David Geffen School of Medicine, University of California Los Angeles
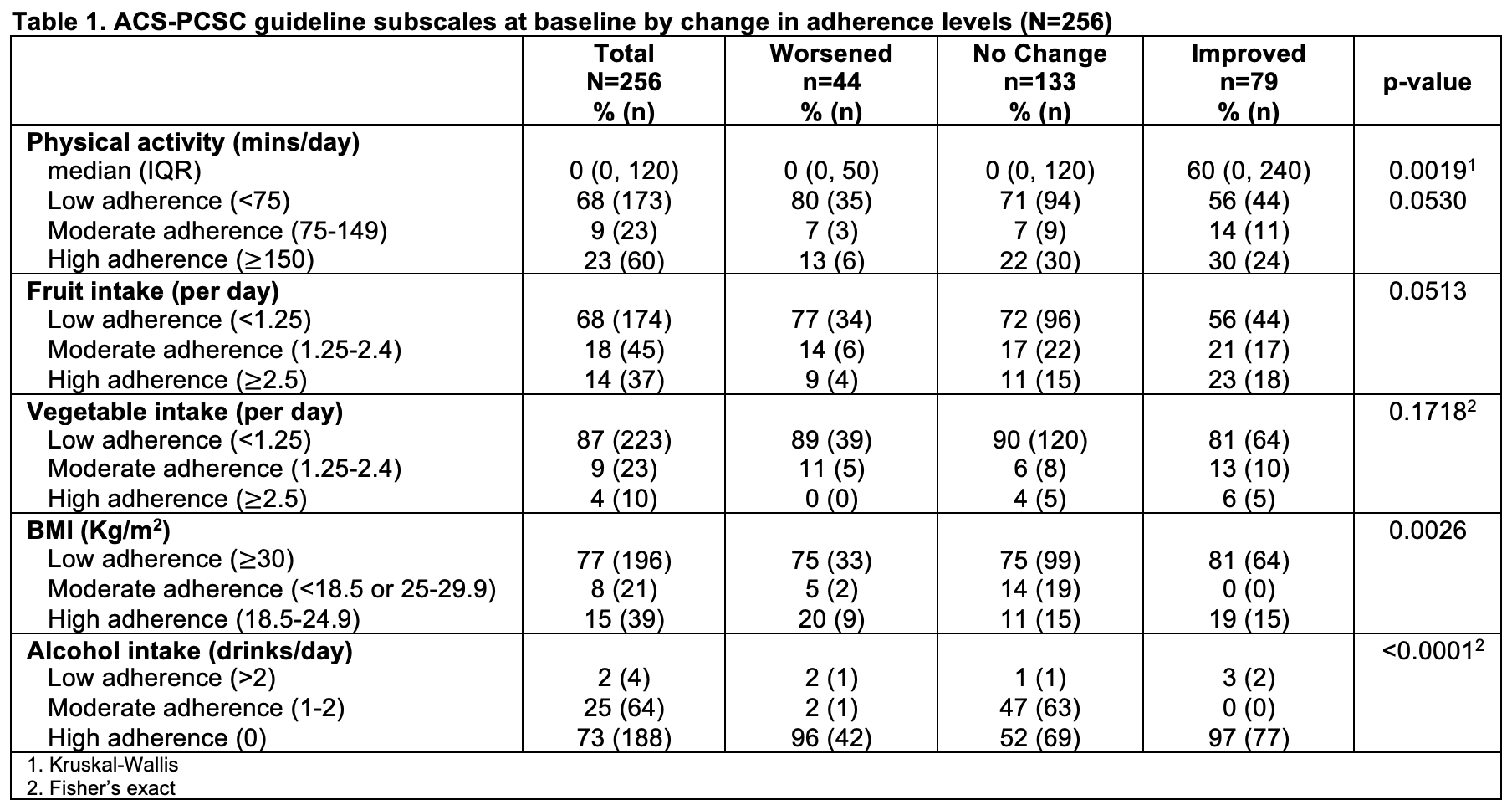
Methods: We retrospectively reviewed survey data from the UCLA Men’s Health Study, a cohort quantifying patient-reported outcomes, and compared baseline surveys collected at program enrollment to 12–18-month follow-up surveys. Five health behavior domains from the California Health Interview Survey were individually and compositely scored based on adherence to the 2014 American Cancer Society Prostate Cancer Survivorship Care (ACS-PCSC) Guidelines. The scores were categorized into three adherence levels: Low, Moderate, and High. Subjects were grouped by change in adherence levels from baseline to follow-up as Worsened, No Change, or Improved. We compared patient demographics, clinical characteristics, health-related quality of life, and adherence to the five domains at baseline between the three groups.
Results: Of the 256 subjects eligible for analysis, 17% worsened, 52% had no change, and 31% improved in overall adherence. Most subjects identified as Hispanic (72%), were foreign born (79%), and had a partner (71%). There were no differences in clinical characteristics among the three adherence change groups. Baseline general and physical health scores were similar, but baseline mental health scores were lower in the worsened group compared to the no change and improved groups (44.3 vs 50.1 vs 47.6, respectively, p=0.0320). Those in the worsened group already had low adherence to physical activity at baseline compared to the no change and improved groups (p=0.0019) (Table 1).
Conclusions: In this cohort of low-income men participating in a free navigation-based prostate cancer treatment program, 31% had improvement in overall adherence to the ACS-PCSC Guidelines for health behaviors. Worsening adherence was associated with lower baseline mental health score and physical activity adherence. Interventions aimed at physical activity may improve overall health behaviors.
Source of Funding: Department of Urology, David Geffen School of Medicine, University of California Los Angeles

.jpg)
.jpg)