Back
Poster, Podium & Video Sessions
Podium
PD25: Health Services Research: Practice Patterns, Quality of Life and Shared Decision Making II
PD25-06: Variation in Communication of Competing Risks of Mortality in Prostate Cancer Treatment Consultations
Saturday, May 14, 2022
10:20 AM – 10:30 AM
Location: Room 244
Aurash Naser-Tavakolian*, Rebecca Gale, Michael Luu, Abhishek Venkataramana, Los Angeles, CA, Dmitry Khodyakov, Santa Monica, CA, Jennifer Anger, Edwin Posadas, Howard Sandler, Brennan Spiegel, Stephen Freedland, Timothy Daskivich, Los Angeles, CA

Aurash NaserTavakolian, MD
Cedars-Sinai Medical Center
Podium Presenter(s)
Introduction: Men with prostate cancer prefer patient-specific, quantitative assessments of longevity in shared decision making. We sought to qualitatively characterize how physicians communicate the three components of competing risks—life expectancy, cancer prognosis, and treatment-related survival benefit—in treatment consultations.
Methods: Conversation related to life expectancy, cancer prognosis, and treatment-related survival benefit was identified in transcripts from treatment consultations of 42 men with low- and intermediate-risk disease across 10 providers (4 urologists, 2 radiation oncologists, and 4 medical oncologists). Consensus of multiple reviewers noted the most detailed mode of communication used to describe each component of competing risks throughout the consultation.
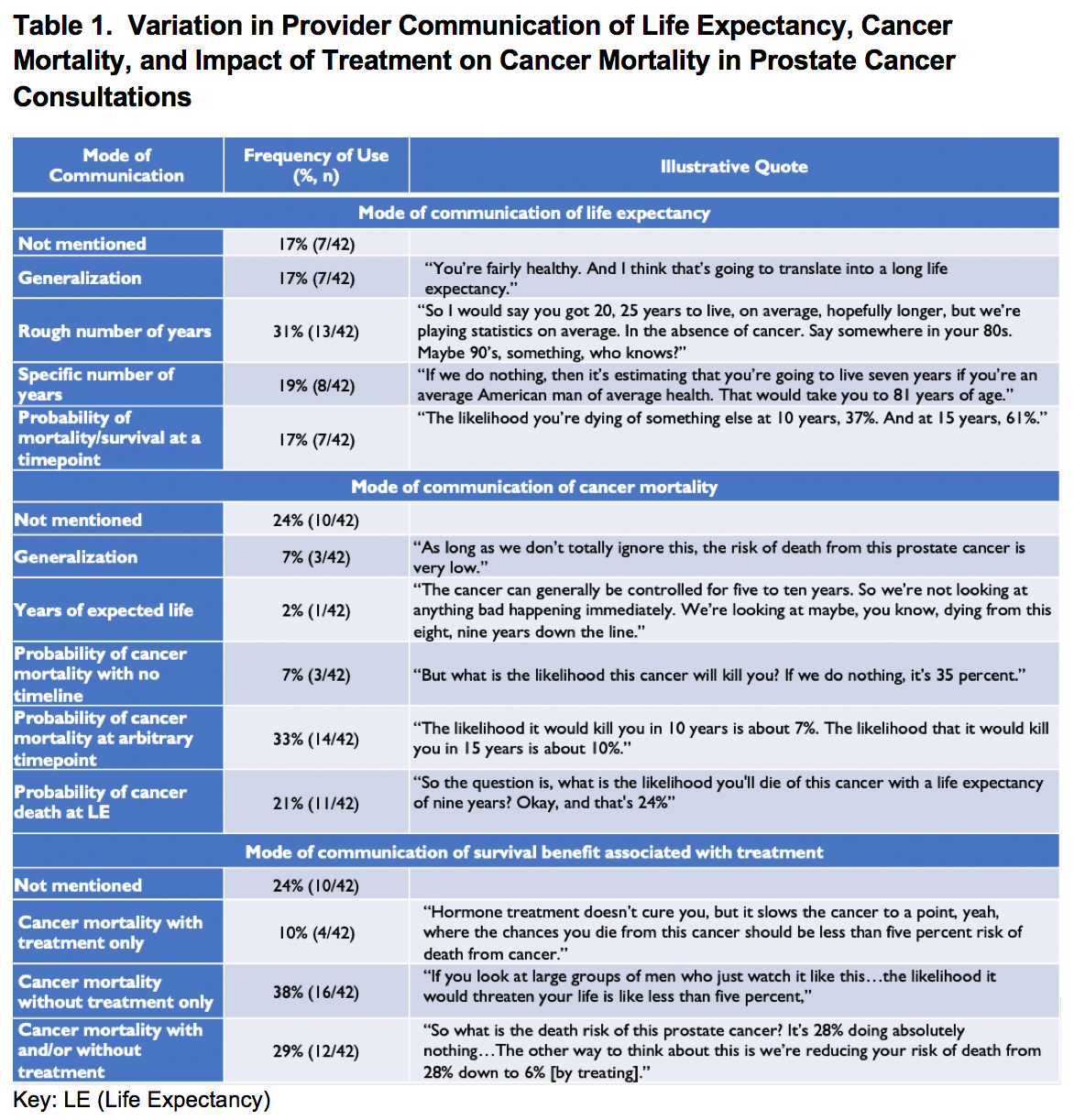
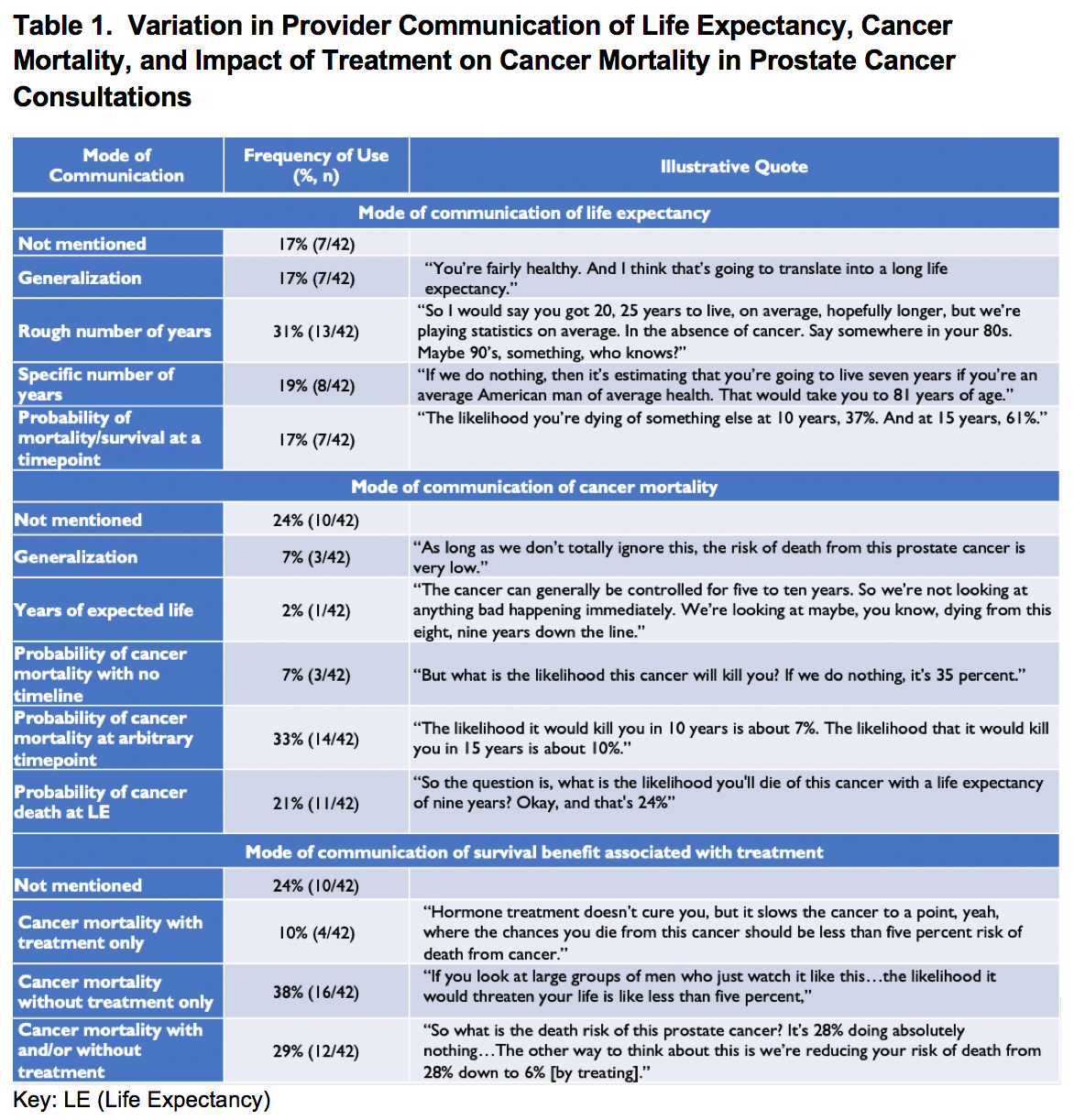
Results: Physicians frequently failed to provide patient-specific, quantitative estimates of both life expectancy and cancer mortality. Life expectancy was omitted in 17% of consultations, expressed as a generalization (e.g. “long”/”short”) in 17%, rough number of years in 31%, probability of mortality/survival at an arbitrary timepoint in 17%, and in only 19% as a specific number of years. Cancer mortality was omitted in 24% of consultations, expressed as a generalization in 7%, years of expected life in 2%, probability at an arbitrary timepoint in 40%, and in only 21% as the probability at the patient’s life expectancy. Treatment-related survival benefit was often omitted; cancer mortality was reported without treatment in 38%, with treatment in 10%, and in only 29% both with and without treatment. Illustrative quotes for these modes of communication are provided in Table 1. Physicians achieved “trifecta”—(1) quantifying probability of cancer mortality (2) with and without treatment (3) at the patient’s life expectancy—in only 14% of consultations.
Conclusions: Physicians often fail to adequately quantify competing risks. We recommend the “trifecta” approach for communicating competing risks, reporting (1) probability of cancer mortality (2) with and without treatment (3) at the patient’s life expectancy.
Source of Funding: This work was supported by Career Development Award (K08 CA230155 to TJD) from the National Cancer Institute.
Methods: Conversation related to life expectancy, cancer prognosis, and treatment-related survival benefit was identified in transcripts from treatment consultations of 42 men with low- and intermediate-risk disease across 10 providers (4 urologists, 2 radiation oncologists, and 4 medical oncologists). Consensus of multiple reviewers noted the most detailed mode of communication used to describe each component of competing risks throughout the consultation.
Results: Physicians frequently failed to provide patient-specific, quantitative estimates of both life expectancy and cancer mortality. Life expectancy was omitted in 17% of consultations, expressed as a generalization (e.g. “long”/”short”) in 17%, rough number of years in 31%, probability of mortality/survival at an arbitrary timepoint in 17%, and in only 19% as a specific number of years. Cancer mortality was omitted in 24% of consultations, expressed as a generalization in 7%, years of expected life in 2%, probability at an arbitrary timepoint in 40%, and in only 21% as the probability at the patient’s life expectancy. Treatment-related survival benefit was often omitted; cancer mortality was reported without treatment in 38%, with treatment in 10%, and in only 29% both with and without treatment. Illustrative quotes for these modes of communication are provided in Table 1. Physicians achieved “trifecta”—(1) quantifying probability of cancer mortality (2) with and without treatment (3) at the patient’s life expectancy—in only 14% of consultations.
Conclusions: Physicians often fail to adequately quantify competing risks. We recommend the “trifecta” approach for communicating competing risks, reporting (1) probability of cancer mortality (2) with and without treatment (3) at the patient’s life expectancy.
Source of Funding: This work was supported by Career Development Award (K08 CA230155 to TJD) from the National Cancer Institute.

.jpg)
.jpg)