Back
Poster, Podium & Video Sessions
Podium
PD27: Prostate Cancer: Localized: Surgical Therapy II
PD27-05: Reliability of 68Ga-PSMA PET/CT in assessing real nodal burden in men with cN1 disease: Clinical implications for patient counselling and multi-modal treatments
Saturday, May 14, 2022
1:40 PM – 1:50 PM
Location: Room 255
Daniele Robesti*, Elio Mazzone, Milano, Italy, Giorgio Gandaglia, Armando Stabile, Milan, Italy, Carlo Andrea Bravi, Andrea Necchi, Daniele Raggi, Laura Marandino, Milano, Italy, Giuseppe Cirulli, Milan, Italy, Nazareno Suardi, Genoa, Italy, Eleonora Balestrazzi, Stefano Fanti, Andrea Farolfi, Lorenzo Bianchi, Bologna, Italy, Shahrokh F. Shariat, Vienna, Austria, Riccardo Schiavina, Bologna, Italy, Francesco Montorsi, Alberto Briganti, Milano, Italy

Daniele Robesti
Vita-Salute San Raffaele University
Podium Presenter(s)
Introduction: 68-Ga PSMA PET/CT demonstrated good accuracy in the primary staging of prostate cancer (PCa). Although previous studies showed a correlation between tumor burden and the risk of PET underestimation for recurrent PCa, no evidence is available for primary staging. Moreover, it is unknown whether the correlation between the number of spots at PSMA PET and the risk of tumor underestimation may be influenced by PSA at imaging.
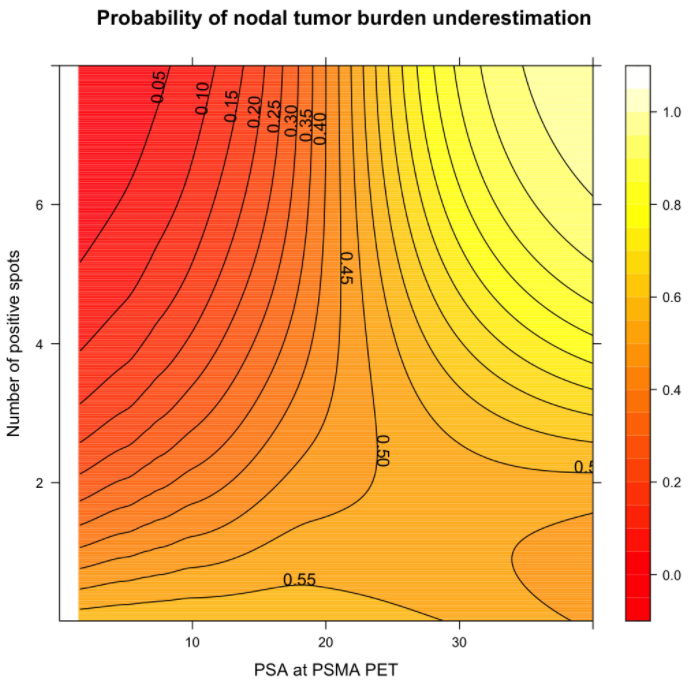
Methods: We identified 92 patients evaluated with 68Ga-PSMA PET/CT before RP and extended lymph node dissection between 2019 and 2021 at two centers. The outcome was tumor underestimation, defined as the difference between the number of positive nodes at pathology and the number of positive nodal spots at PSMA PET/CT. Multivariable linear regression analyses tested the association between number of positive spots at PSMA PET and underestimation of tumor burden. The continuous interaction between preoperative PSA and number of positive spots and the probability of tumor underestimation was graphically explored through an heatmap.
Results: Median PSA at scan was 9 ng/ml (IQR 5-16 ng/ml). Overall, 30 patients (32%) had positive nodal spots at PSMA PET while 32 (35%) had histologically confirmed positive nodes. Of men with nodal spots at PSMA PET, 19/30 (63%) had pN1 disease with a specificity of 81%. Among patients with positive PET, the median number of positive spots was 2 (IQR 1-3). PSMA PET underestimated the burden of nodal invasion in 22 of 30 men with positive spots (73%). Patients with underestimated nodal burden had higher rate of PSA persistence (36%) compared with those without underestimation (11%). In linear regression analyses, higher number of positive spots was associated with increased risk of underestimating tumoral burden (OR 1.05, p=0.02). When graphically explored, the underestimation rate progressively increased with higher PSA level and higher tumor burden at PET.
Conclusions: PSMA PET underestimates the real tumor burden in men with cN1 disease. Higher number of positive spots is associated with increased risk of tumor underestimation. Our data suggest that patients with high PSA level and high number of positive spots might have upfront disseminated disease and thus are more suitable for multi-modal approach.
Source of Funding: None.
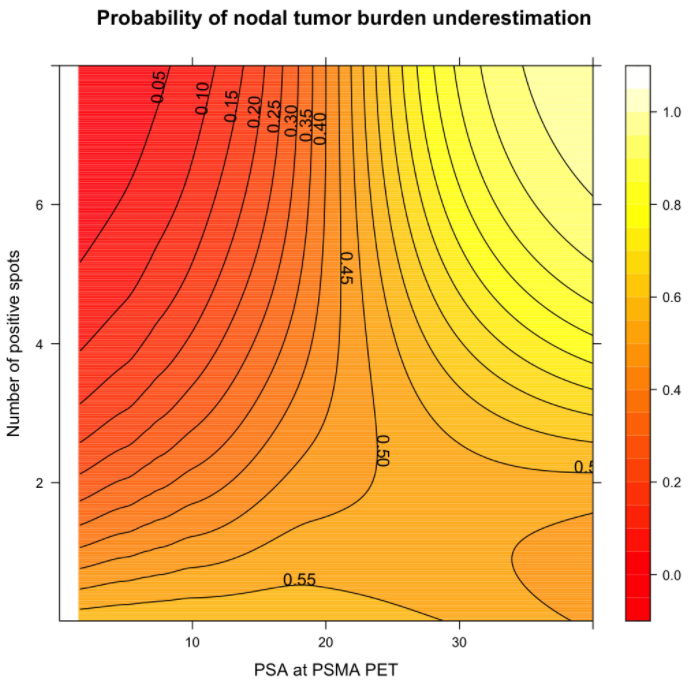
Methods: We identified 92 patients evaluated with 68Ga-PSMA PET/CT before RP and extended lymph node dissection between 2019 and 2021 at two centers. The outcome was tumor underestimation, defined as the difference between the number of positive nodes at pathology and the number of positive nodal spots at PSMA PET/CT. Multivariable linear regression analyses tested the association between number of positive spots at PSMA PET and underestimation of tumor burden. The continuous interaction between preoperative PSA and number of positive spots and the probability of tumor underestimation was graphically explored through an heatmap.
Results: Median PSA at scan was 9 ng/ml (IQR 5-16 ng/ml). Overall, 30 patients (32%) had positive nodal spots at PSMA PET while 32 (35%) had histologically confirmed positive nodes. Of men with nodal spots at PSMA PET, 19/30 (63%) had pN1 disease with a specificity of 81%. Among patients with positive PET, the median number of positive spots was 2 (IQR 1-3). PSMA PET underestimated the burden of nodal invasion in 22 of 30 men with positive spots (73%). Patients with underestimated nodal burden had higher rate of PSA persistence (36%) compared with those without underestimation (11%). In linear regression analyses, higher number of positive spots was associated with increased risk of underestimating tumoral burden (OR 1.05, p=0.02). When graphically explored, the underestimation rate progressively increased with higher PSA level and higher tumor burden at PET.
Conclusions: PSMA PET underestimates the real tumor burden in men with cN1 disease. Higher number of positive spots is associated with increased risk of tumor underestimation. Our data suggest that patients with high PSA level and high number of positive spots might have upfront disseminated disease and thus are more suitable for multi-modal approach.
Source of Funding: None.

.jpg)
.jpg)