Back
Poster, Podium & Video Sessions
Podium
PD27: Prostate Cancer: Localized: Surgical Therapy II
PD27-07: Prostate Volume, Baseline Urinary Symptoms, and Their Association with Post-Treatment Urinary Function in Men Treated for Localized Prostate Cancer
Saturday, May 14, 2022
2:00 PM – 2:10 PM
Location: Room 255
Jacob Tallman*, Christopher Wallis, Li-Ching Huang, Zhiguo Zhao, David Penson, Tatsuki Koyama, Ralph Conwill, Nashville, TN, Michael Goodman, Atlanta, GA, Ann Hamilton, Los Angeles, CA, Xiao-Cheng Wu, New Orleans, LA, Lisa Paddock, Antoinette Stroup, New Brunswick, NJ, Matthew Cooperberg, San Francisco, CA, Mia Hashibe, Brock O'Neil, Salt Lake City, UT, Sherrie Kaplan, Sheldon Greenfield, Irvine, CA, Karen Hoffman, Houston, TX, Daniel Barocas, Nashville, TN

Jacob E. Tallman, MD (he/him/his)
Memorial Sloan-Kettering Cancer Center
Podium Presenter(s)
Introduction: While a patient’s prostate volume (PV) and baseline lower urinary tract symptoms (LUTS) often contribute to decision-making in men with localized PCa, it is unknown to what degree PV and LUTS are associated with treatment choice and post-treatment urinary function. We hypothesized that larger PV and worse baseline LUTS would be associated with choosing surgery or active surveillance over radiation therapy (RT) and with larger improvement in urinary symptoms after treatment.
Methods: CEASAR is a prospective cohort study that enrolled men with localized PCa from 2011-2012. 1823 men who completed both baseline and post-treatment surveys were included. Patient-reported health-related quality of life (HRQOL) was evaluated using the Expanded Prostate Index Composite (EPIC-26) with up to 5 years follow up. Men were grouped by PV (0-30cc, 31-50, 51-70, and 70+) and baseline LUTS (urinary irritative domain score 0-75, 76-85, 86-95, and 95-100). We evaluated the association of baseline PV and LUTS with post-treatment urinary function using multivariable analyses.
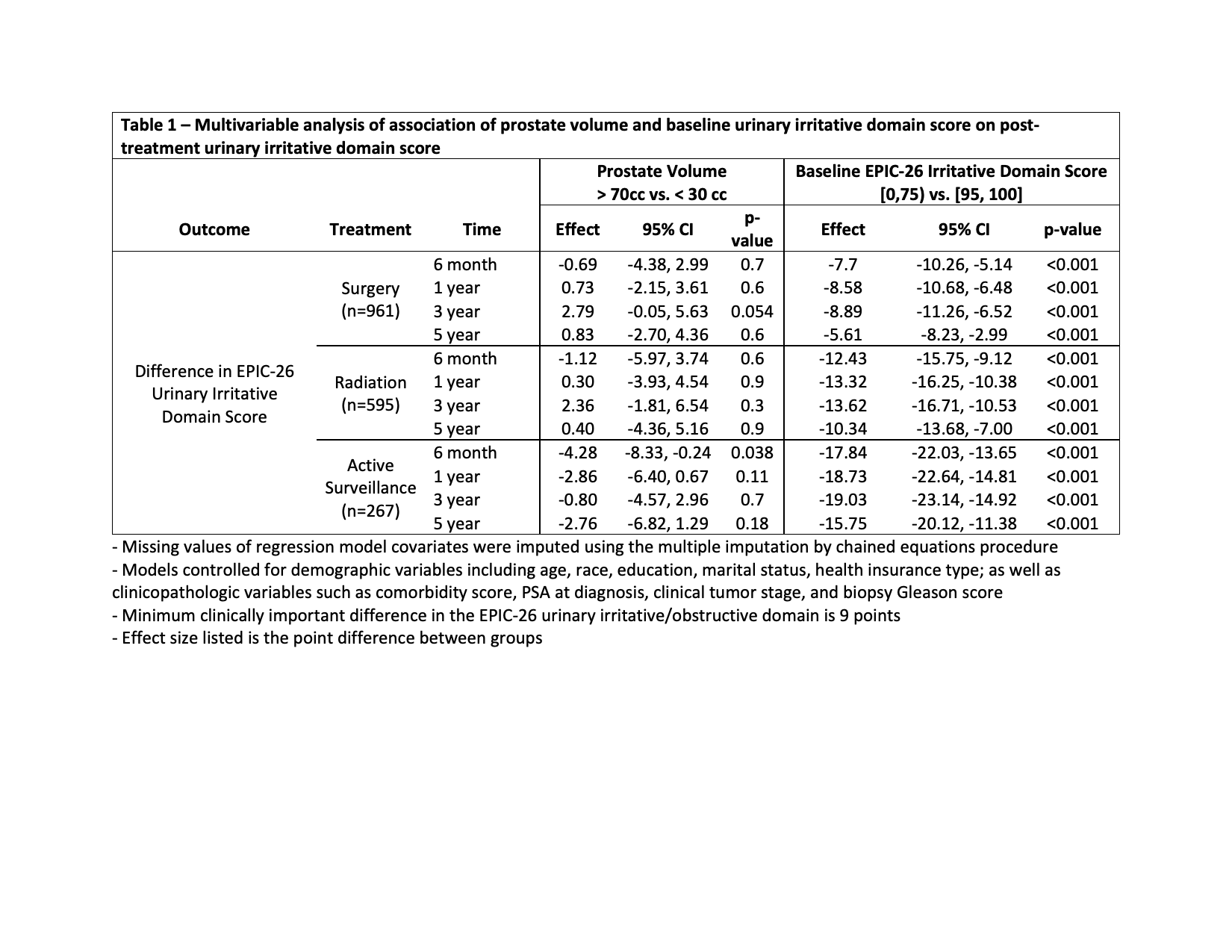
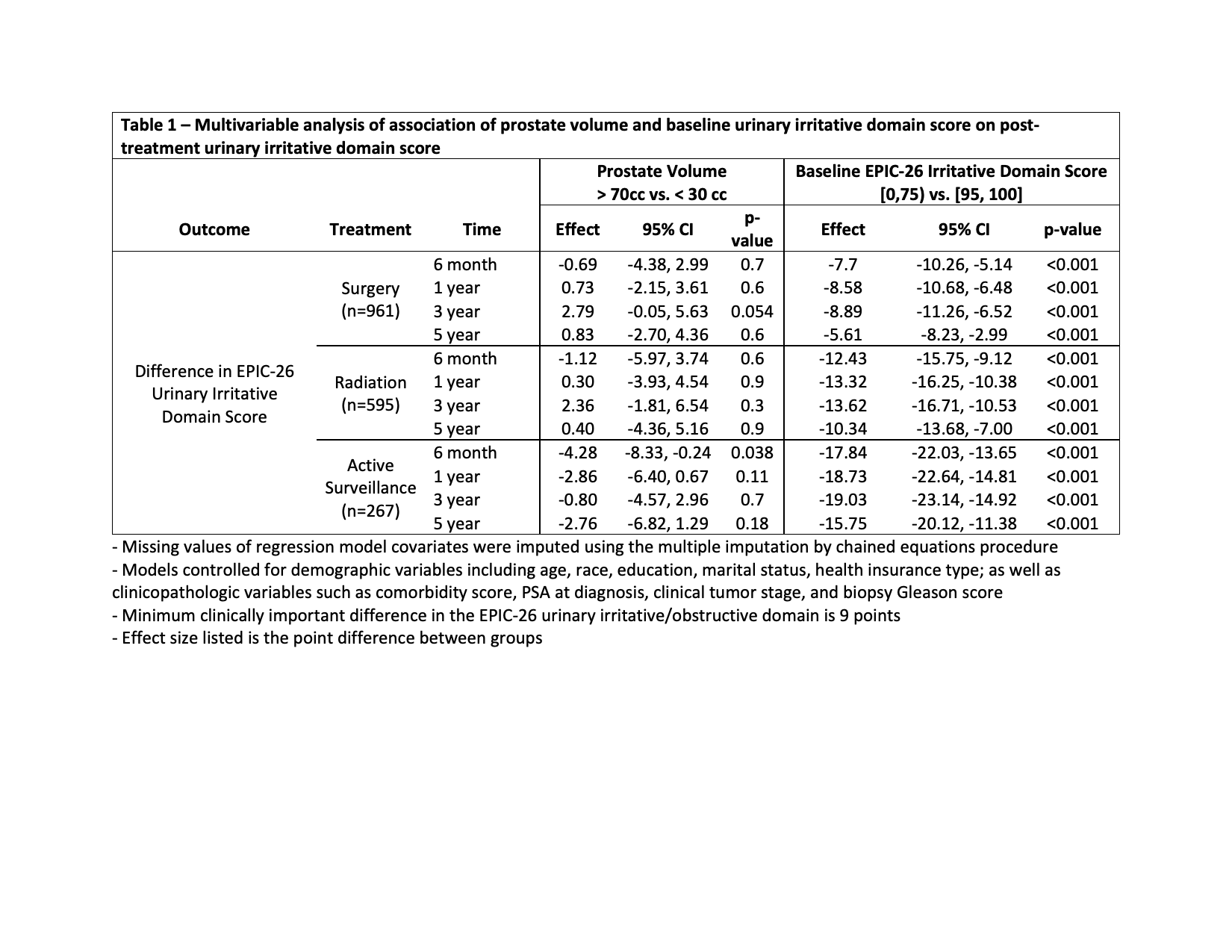
Results: Median age was 64 (IQR 59-69) years. 896 (51%) had grade group 1 PCa and 485 (28%) grade group 2. 961 (53%) received surgery, 595 (33%) RT, and 267 (14%) active surveillance. Larger PV was weakly associated with worse LUTS at baseline (R = -0.17; p < 0.001). On multivariable analysis by PV, there were no clinically significant differences in treatment choice or post-treatment LUTS. Men with optimal baseline urinary function had less LUTS post-treatment compared to men with worse baseline function (Table 1). Men with poor baseline LUTS saw improvement post-treatment; surgery led to greater improvement than RT. These differences meet the minimum clinically important difference (9 points). Subgroup analysis excluding androgen deprivation therapy use had no significant impact on the results.
Conclusions: While baseline PV had no significant association with post-treatment LUTS, worse baseline LUTS were associated with significantly worse LUTS after treatment with a durable effect out to 5 years. Men with poor LUTS tend to improve with treatment, more so with surgery than RT. Urologists should consider patient’s baseline LUTS when counseling about treatment options for PCa.
Source of Funding: AHRQ: 1R01HS019356, 1R01HS022640. PCORI: CE-12-11-4667. NCI: 5T32CA106183, R01CA230352. NCATS: UL1TR000011
Methods: CEASAR is a prospective cohort study that enrolled men with localized PCa from 2011-2012. 1823 men who completed both baseline and post-treatment surveys were included. Patient-reported health-related quality of life (HRQOL) was evaluated using the Expanded Prostate Index Composite (EPIC-26) with up to 5 years follow up. Men were grouped by PV (0-30cc, 31-50, 51-70, and 70+) and baseline LUTS (urinary irritative domain score 0-75, 76-85, 86-95, and 95-100). We evaluated the association of baseline PV and LUTS with post-treatment urinary function using multivariable analyses.
Results: Median age was 64 (IQR 59-69) years. 896 (51%) had grade group 1 PCa and 485 (28%) grade group 2. 961 (53%) received surgery, 595 (33%) RT, and 267 (14%) active surveillance. Larger PV was weakly associated with worse LUTS at baseline (R = -0.17; p < 0.001). On multivariable analysis by PV, there were no clinically significant differences in treatment choice or post-treatment LUTS. Men with optimal baseline urinary function had less LUTS post-treatment compared to men with worse baseline function (Table 1). Men with poor baseline LUTS saw improvement post-treatment; surgery led to greater improvement than RT. These differences meet the minimum clinically important difference (9 points). Subgroup analysis excluding androgen deprivation therapy use had no significant impact on the results.
Conclusions: While baseline PV had no significant association with post-treatment LUTS, worse baseline LUTS were associated with significantly worse LUTS after treatment with a durable effect out to 5 years. Men with poor LUTS tend to improve with treatment, more so with surgery than RT. Urologists should consider patient’s baseline LUTS when counseling about treatment options for PCa.
Source of Funding: AHRQ: 1R01HS019356, 1R01HS022640. PCORI: CE-12-11-4667. NCI: 5T32CA106183, R01CA230352. NCATS: UL1TR000011

.jpg)
.jpg)