Back
Poster, Podium & Video Sessions
Podium
PD27: Prostate Cancer: Localized: Surgical Therapy II
PD27-08: Predictors and trends of opioid-sparing radical prostatectomy from a large national cohort
Saturday, May 14, 2022
2:10 PM – 2:20 PM
Location: Room 255
Aaron Brant, Patrick Lewicki, Alec Zhu*, Christina Sze, Jeffrey Johnson, Christopher Gaffney, New York, NY, Ilon Weinstein, Anise Bowman, Jonathan Shoag, Cleveland, OH

Alec Zhu, MD, BA
Weill Cornell-NewYork Presbyterian
Podium Presenter(s)
Introduction: Amidst a nationwide opioid epidemic, multiple urologic societies have published guidelines to encourage judicious use of opioids after urologic surgery. We used a large national database to examine trends in use of opioid and non-opioid pain medications after radical prostatectomy.
Methods: The Premier Hospital Database was queried to identify all robotic and/or laparoscopic radical prostatectomies (RALP) from 2015 – 2020 with length of stay =1 day. “Opioid-sparing” was defined as absence of intravenous opioid use after post-operative day 0 and absence of oral opioid use throughout admission. Comparisons were made between opioid-sparing and non-opioid-sparing RALPs. Logistic multivariable regression was used to identify predictors of opioid-sparing RALP. Trends of opioid prescribing patterns over time were plotted, as were density plots of surgeon prescribing behavior.
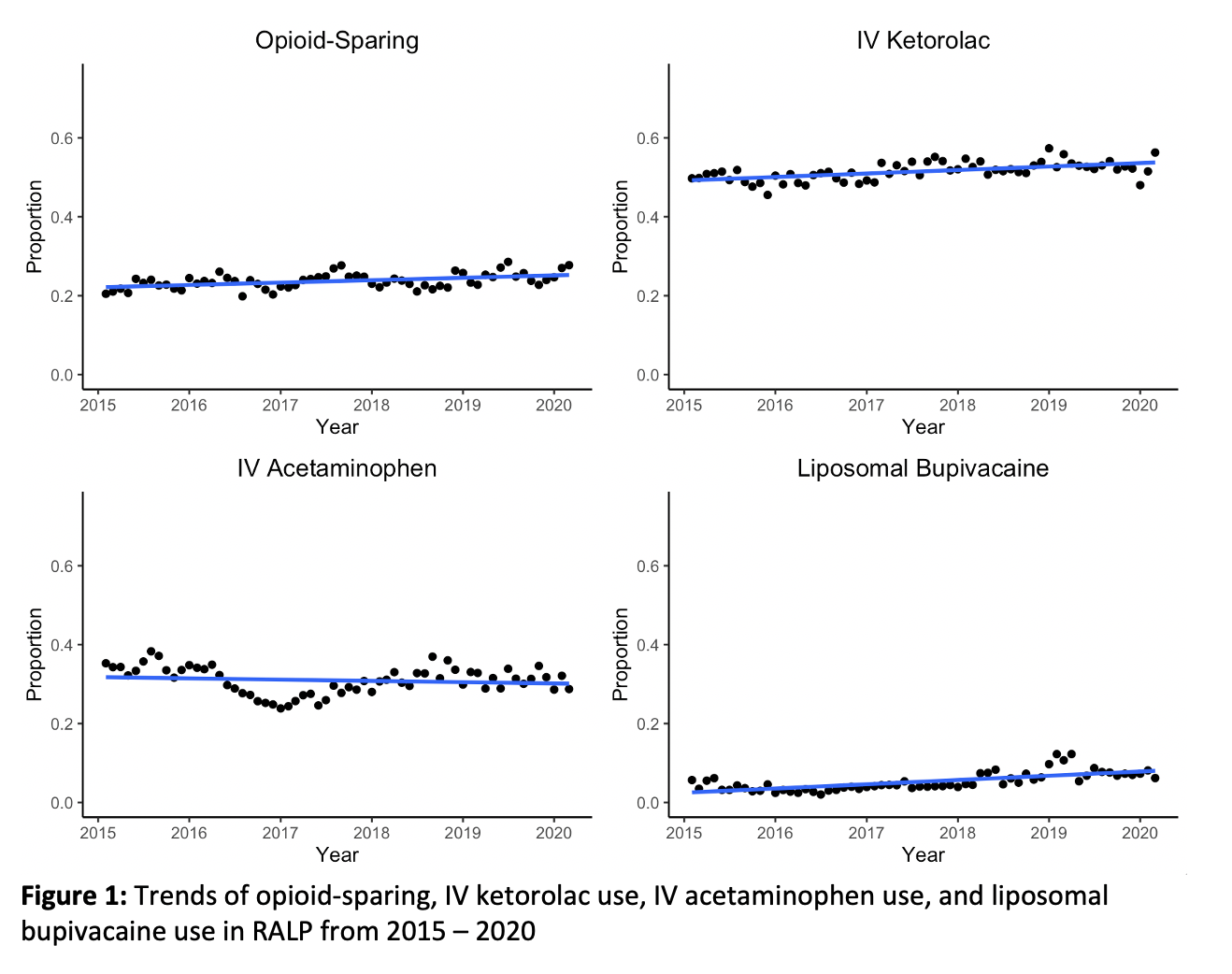
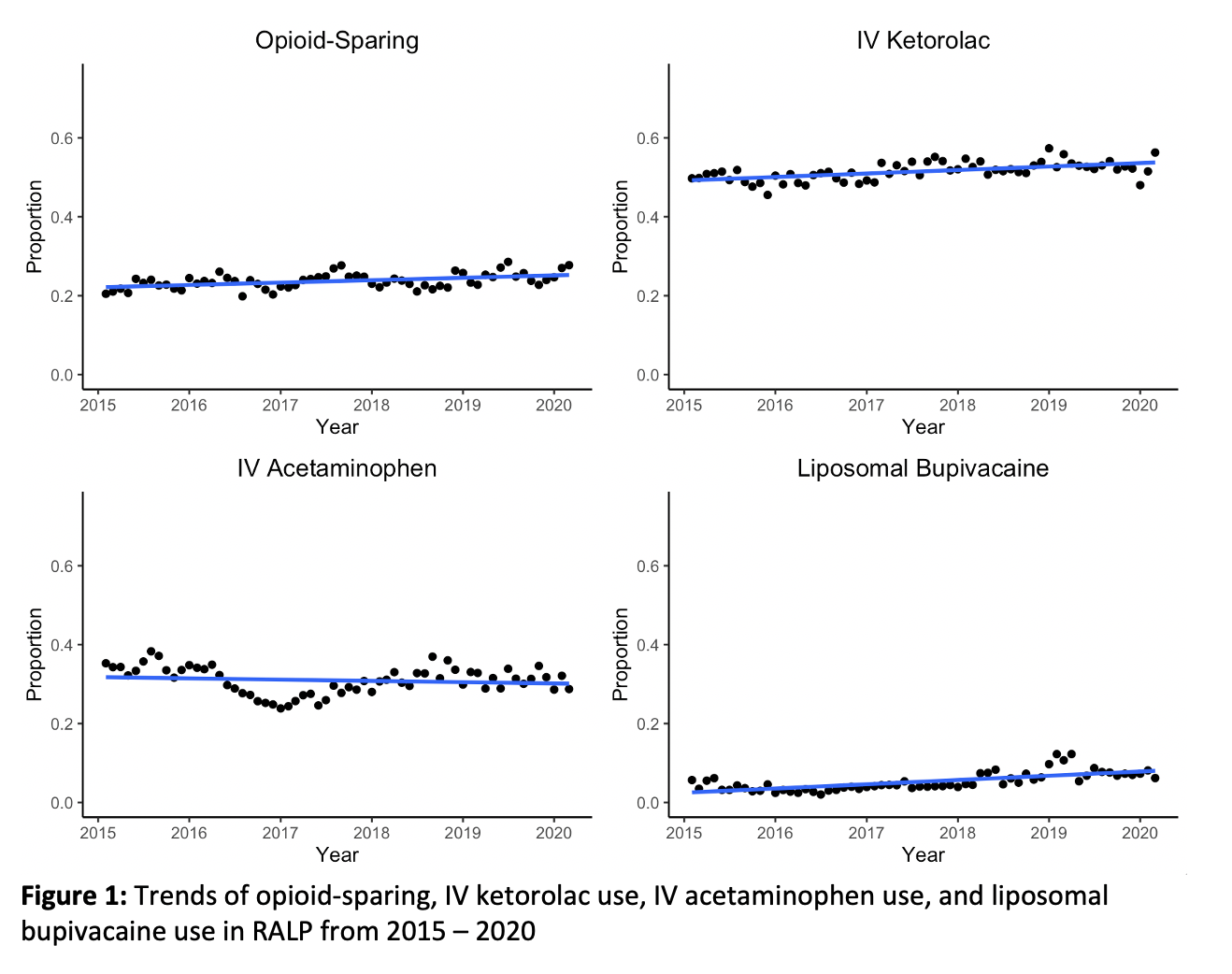
Results: A total of 62,728 patients met inclusion criteria. The overall opioid-sparing rate was 24%. Opioid-sparing RALPs were associated with older age (65 vs. 63 years, p<0.01), white race (76.3% vs. 73.3%, p<0.01), high-volume surgeons (75.2% vs. 70.0%, p<0.01), IV ketorolac (62.2% vs. 48.0%, p<0.01), IV acetaminophen (32.5% vs. 30.0%, p<0.01), and liposomal bupivacaine (5.4% vs. 4.9%, p<0.01). On multivariable regression, IV ketorolac was the strongest predictor of opioid-sparing RALP (OR 1.77 [1.71 – 1.83], p<0.01). The proportion of procedures that used IV ketorolac, liposomal bupivacaine, and were opioid-sparing increased in frequency over time, while the proportion that used IV acetaminophen decreased (Figure 1). IV ketorolac was not associated with increased postoperative bleeding (0.3% vs. 0.3%, p=0.9) or inpatient dialysis ( <0.1% vs. <0.1%, p=0.8). Density plots of ketorolac prescribing behavior showed a bimodal distribution with the majority of providers either frequently (>75%) or infrequently ( <25%) prescribing ketorolac.
Conclusions: Opioid-sparing RALP was associated with IV ketorolac, IV acetaminophen, and liposomal bupivacaine use. On multivariable regression, IV ketorolac was the strongest predictor of opioid-sparing RALP and was not associated with increased risk of bleeding or dialysis. There were large discrepancies in ketorolac prescribing behavior among urologists.
Source of Funding: None
Methods: The Premier Hospital Database was queried to identify all robotic and/or laparoscopic radical prostatectomies (RALP) from 2015 – 2020 with length of stay =1 day. “Opioid-sparing” was defined as absence of intravenous opioid use after post-operative day 0 and absence of oral opioid use throughout admission. Comparisons were made between opioid-sparing and non-opioid-sparing RALPs. Logistic multivariable regression was used to identify predictors of opioid-sparing RALP. Trends of opioid prescribing patterns over time were plotted, as were density plots of surgeon prescribing behavior.
Results: A total of 62,728 patients met inclusion criteria. The overall opioid-sparing rate was 24%. Opioid-sparing RALPs were associated with older age (65 vs. 63 years, p<0.01), white race (76.3% vs. 73.3%, p<0.01), high-volume surgeons (75.2% vs. 70.0%, p<0.01), IV ketorolac (62.2% vs. 48.0%, p<0.01), IV acetaminophen (32.5% vs. 30.0%, p<0.01), and liposomal bupivacaine (5.4% vs. 4.9%, p<0.01). On multivariable regression, IV ketorolac was the strongest predictor of opioid-sparing RALP (OR 1.77 [1.71 – 1.83], p<0.01). The proportion of procedures that used IV ketorolac, liposomal bupivacaine, and were opioid-sparing increased in frequency over time, while the proportion that used IV acetaminophen decreased (Figure 1). IV ketorolac was not associated with increased postoperative bleeding (0.3% vs. 0.3%, p=0.9) or inpatient dialysis ( <0.1% vs. <0.1%, p=0.8). Density plots of ketorolac prescribing behavior showed a bimodal distribution with the majority of providers either frequently (>75%) or infrequently ( <25%) prescribing ketorolac.
Conclusions: Opioid-sparing RALP was associated with IV ketorolac, IV acetaminophen, and liposomal bupivacaine use. On multivariable regression, IV ketorolac was the strongest predictor of opioid-sparing RALP and was not associated with increased risk of bleeding or dialysis. There were large discrepancies in ketorolac prescribing behavior among urologists.
Source of Funding: None

.jpg)
.jpg)