Back
Poster, Podium & Video Sessions
Podium
PD30: Education Research III
PD30-01: Observed differences in urology resident operative autonomy associated with patient race
Saturday, May 14, 2022
1:00 PM – 1:10 PM
Location: Room 243
Anh Nguyen*, Jacob Veliky, John Fastenau, Newark, NJ, Devashish Anjaria, Joseph Oliver, Anastasia Kunac, Hossein Sadeghi-Nejad, East Orange, NJ

Anh T. Nguyen, MD
Rutgers NJMS
Podium Presenter(s)
Introduction: Surgical resident operative autonomy is a topic of interest due to findings of decreased confidence and preparedness of graduates. It has been observed that autonomy afforded to general surgery residents is not equal across patient races. This study seeks to determine if there are differences in urology resident operative autonomy associated with patient race.
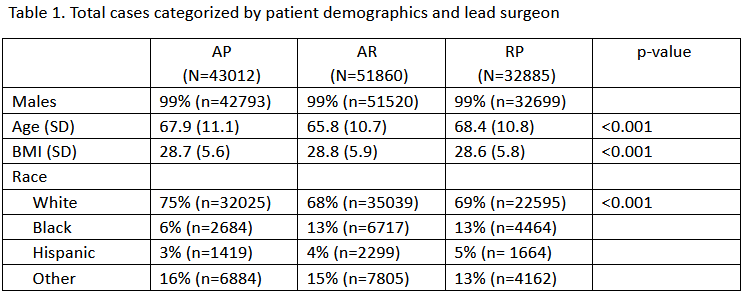
Methods: The VA Surgical Quality Improvement Program (VASQIP) was queried for the top five urologic procedures between 2004 to 2019 at teaching VA hospitals. The most common resident performed cases within the database were transurethral resection of prostate, transurethral resection (small, medium, or large tumor), GreenLight laser of prostate, hydrocelectomy, and ureteral stent placement. The cases were stratified by attending supervision: attending as primary surgeon (AP), attending and resident (AR), resident as primary surgeon with the attending not scrubbed (RP). We compared patient demographic data including age, BMI, and race between resident supervision levels utilizing Anova for continuous data and Chi Squared for categorical data.
Results: 127,757 urology cases were identified from 2004 to 2019. The above procedures accounted for 76.5% of all urologic cases performed at the VA. All demographics were significantly different (p < 0.001) There was a lower percentage of white patients in the RP and AR categories compared to AP (69% vs 68% vs 75%) and nearly double the percentage of black patients (13% vs 13% vs 6%). (Table 1).
Conclusions: Urology residents were significantly more likely to be afforded operative autonomy on minority patients, while white patients were significantly more likely to have an attending surgeon as the primary surgeon. This observation is similar to that seen in general surgery and requires in depth analysis to assess if this is due to bias versus an observed difference secondary to geographical differences in patient demographics at high volume VA medical centers.
Source of Funding: none
Methods: The VA Surgical Quality Improvement Program (VASQIP) was queried for the top five urologic procedures between 2004 to 2019 at teaching VA hospitals. The most common resident performed cases within the database were transurethral resection of prostate, transurethral resection (small, medium, or large tumor), GreenLight laser of prostate, hydrocelectomy, and ureteral stent placement. The cases were stratified by attending supervision: attending as primary surgeon (AP), attending and resident (AR), resident as primary surgeon with the attending not scrubbed (RP). We compared patient demographic data including age, BMI, and race between resident supervision levels utilizing Anova for continuous data and Chi Squared for categorical data.
Results: 127,757 urology cases were identified from 2004 to 2019. The above procedures accounted for 76.5% of all urologic cases performed at the VA. All demographics were significantly different (p < 0.001) There was a lower percentage of white patients in the RP and AR categories compared to AP (69% vs 68% vs 75%) and nearly double the percentage of black patients (13% vs 13% vs 6%). (Table 1).
Conclusions: Urology residents were significantly more likely to be afforded operative autonomy on minority patients, while white patients were significantly more likely to have an attending surgeon as the primary surgeon. This observation is similar to that seen in general surgery and requires in depth analysis to assess if this is due to bias versus an observed difference secondary to geographical differences in patient demographics at high volume VA medical centers.
Source of Funding: none

.jpg)
.jpg)