Back
Poster, Podium & Video Sessions
Podium
PD30: Education Research III
PD30-11: Characterization of Gender Differences in H-Index within Urologic Subspecialties
Saturday, May 14, 2022
2:40 PM – 2:50 PM
Location: Room 243
Bridget Findlay*, Rochester, MN, Timothy Lyon, Jacksonville, FL, Maraika Robinson, Elizabeth Bearrick, Boyd Viers, Rochester, MN, Colleen Ball, Jacksonville, FL, Katherine Anderson, Rochester, MN
- BF
Bridget Lang Findlay, MD, BS (she/her/hers)
Resident
Mayo Clinic, Rochester, MN
Podium Presenter(s)
Introduction: H-index is a bibliometric measure used to quantify an individual’s scholarly productivity. Male urologists have higher h-indices than women and proportionally achieve more senior academic rank; however, the degree to which h-indices may vary by gender within urologic subspecialties has not been well defined. Recognizing that more granular h-index benchmarks may help promote gender equity in academic advancement, we aim to assess differences in h-index between genders amongst different subspecialties.
Methods: A list of academic urologists was generated using AUA-accredited residency program websites as of July 2021. Gender, subspecialty, AUA section, and academic rank were recorded. Scopus was queried to identify h-indices. Descriptive statistics were performed for the entire group and within subspecialties (oncology, endourology, pediatrics, FPMRS, andrology, reconstruction, general urology). Univariable and multivariable linear regression models were created to characterize the relationship between h-index and gender.
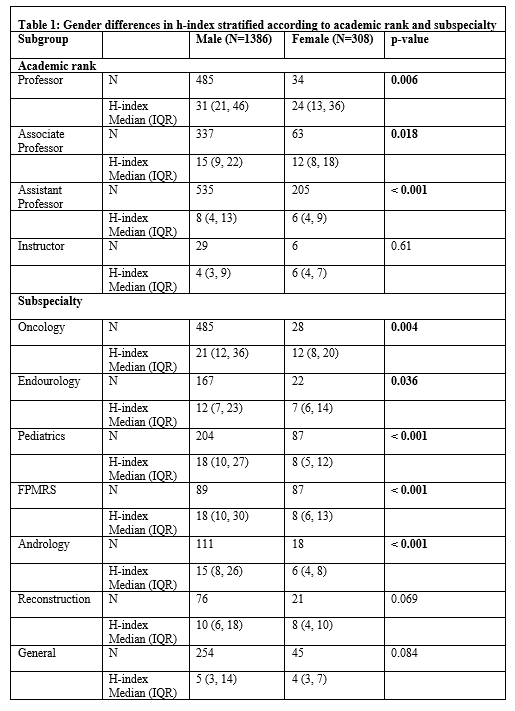
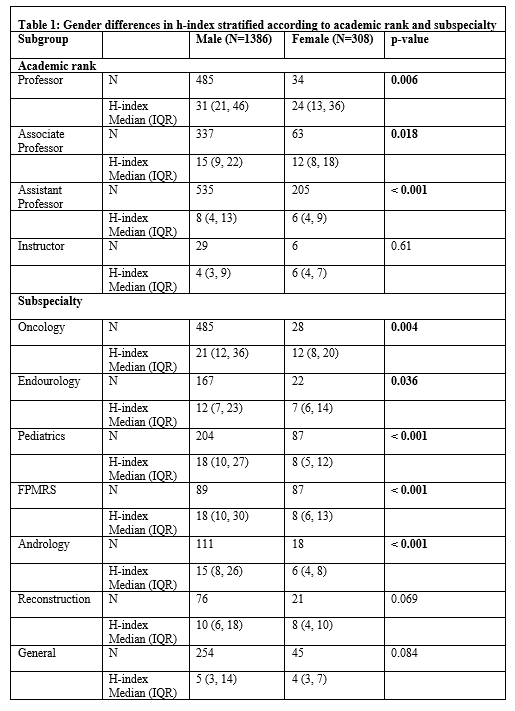
Results: A total of 1694 academic urologists from 137 AUA-accredited institutions were included, of whom 308 were women (18.2%). Oncology was the most common subspecialty; however, it contained the smallest proportion of women (5.6%, 28/513). Subspecialties with the highest proportion of women included FPMRS (49%, 87/716) and pediatric urology (30%, 87/291). Overall, mean h-index for women was lower than for men (adjusted mean difference -10.1, 95% CI -12.2 to -8.0, p<0.001) Men had significantly higher h-indices across all academic ranks except instructor, all subspecialties except reconstruction and general urology, and across all AUA sections except Northeast section (Table 1). After adjusting for MD/PhD status, subspecialty, year since first publication, and AUA section, h-index was significantly lower for women by an average of 2.2 points (p=0.03).
Conclusions: Male urologists have significantly higher h-indices than women even after adjusting for academic rank, subspecialty, and geographic region. The use of gender- and subspecialty-specific h-index metrics to guide academic advancement decisions may be a useful strategy to promote gender equity in academic urology.
Source of Funding: N/A
Methods: A list of academic urologists was generated using AUA-accredited residency program websites as of July 2021. Gender, subspecialty, AUA section, and academic rank were recorded. Scopus was queried to identify h-indices. Descriptive statistics were performed for the entire group and within subspecialties (oncology, endourology, pediatrics, FPMRS, andrology, reconstruction, general urology). Univariable and multivariable linear regression models were created to characterize the relationship between h-index and gender.
Results: A total of 1694 academic urologists from 137 AUA-accredited institutions were included, of whom 308 were women (18.2%). Oncology was the most common subspecialty; however, it contained the smallest proportion of women (5.6%, 28/513). Subspecialties with the highest proportion of women included FPMRS (49%, 87/716) and pediatric urology (30%, 87/291). Overall, mean h-index for women was lower than for men (adjusted mean difference -10.1, 95% CI -12.2 to -8.0, p<0.001) Men had significantly higher h-indices across all academic ranks except instructor, all subspecialties except reconstruction and general urology, and across all AUA sections except Northeast section (Table 1). After adjusting for MD/PhD status, subspecialty, year since first publication, and AUA section, h-index was significantly lower for women by an average of 2.2 points (p=0.03).
Conclusions: Male urologists have significantly higher h-indices than women even after adjusting for academic rank, subspecialty, and geographic region. The use of gender- and subspecialty-specific h-index metrics to guide academic advancement decisions may be a useful strategy to promote gender equity in academic urology.
Source of Funding: N/A

.jpg)
.jpg)