Back
Poster, Podium & Video Sessions
Podium
PD30: Education Research III
PD30-12: Comparison of Urogynecological Training Among US Urology and Obstetrics and Gynecology Residents and the Impact FPMRS fellowship and dedicated rotation time have on training
Saturday, May 14, 2022
2:50 PM – 3:00 PM
Location: Room 243
Michael Hung, Ashley Huber, Rosen Jeong*, Jason Kim, Stony Brook, NY
- RJ
Podium Presenter(s)
Introduction: Board certified Female Pelvic Medicine and Reconstructive Surgeons (FPRMS) include physicians from both obstetrics and gynecology (Ob/Gyn) and urology backgrounds. We sought to explore differences in experiences and comfort level for common FPMRS procedures between both training programs. A secondary goal was to examine the impact of a FPMRS rotation or presence of FPMRS fellowship.
Methods: We created and distributed an anonymous, IRB approved, survey to residents graduating in 2020. The survey assessed general case numbers and self-rated comfort with performing a given procedure. Comparisons between Ob/Gyn and urology residents for each procedure was performed using Mann-Whitney U tests.
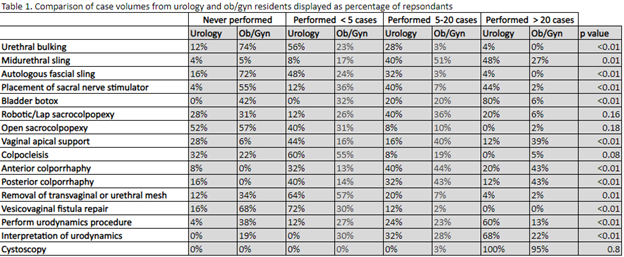
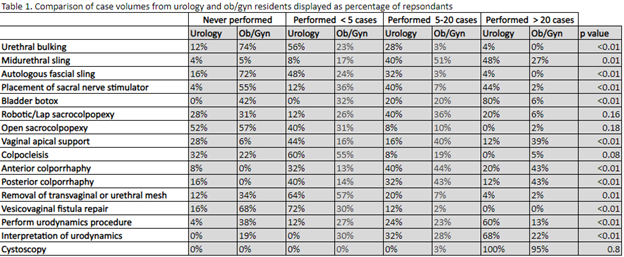
Results: Responses were recorded from 6.6% (n=90) of Ob/Gyn residents and 7.7% (n=25) of urology. Ob/Gyn residents performed significantly more vaginal apical support and anterior/posterior colporrhaphies compared to urology residents(p < 0.01). Urology residents performed more urethral bulking, midurethral slings, autologous fascial slings, sacral nerve stimulators, bladder botox, vesicovaginal fistula repairs, and urodynamics(p < 0.01). Ob/Gyn and Urology programs were noted to have an associated FPMRS fellowship 22% (n= 20) and 24% (n=6) of the time, respectively. There was no statistical difference in the training of Urology residents at programs with or without fellowship. Ob/Gyn residents at programs with fellowships were found to have more exposure to autologous slings (0.62 vs 0.24 p=0.004) but less exposure to midurethral slings (1.44 vs 2.18 p=0.001) and vaginal apical support (2.21 vs 1.72 p=0.025).
Conclusions: A comprehensive picture of resident’s experience with FPMRS procedures suggest that urology residents have more experience, and overall, more comfort with performing many common FPMRS procedures without formal fellowship training. However, it is notable that Ob/Gyn residents have significantly more experience and comfort with transvaginal procedures. Additionally, there is minimal impact of a fellowship and dedicated rotation in the exposure/comfort to FPMRS procedures.
Source of Funding: None
Methods: We created and distributed an anonymous, IRB approved, survey to residents graduating in 2020. The survey assessed general case numbers and self-rated comfort with performing a given procedure. Comparisons between Ob/Gyn and urology residents for each procedure was performed using Mann-Whitney U tests.
Results: Responses were recorded from 6.6% (n=90) of Ob/Gyn residents and 7.7% (n=25) of urology. Ob/Gyn residents performed significantly more vaginal apical support and anterior/posterior colporrhaphies compared to urology residents(p < 0.01). Urology residents performed more urethral bulking, midurethral slings, autologous fascial slings, sacral nerve stimulators, bladder botox, vesicovaginal fistula repairs, and urodynamics(p < 0.01). Ob/Gyn and Urology programs were noted to have an associated FPMRS fellowship 22% (n= 20) and 24% (n=6) of the time, respectively. There was no statistical difference in the training of Urology residents at programs with or without fellowship. Ob/Gyn residents at programs with fellowships were found to have more exposure to autologous slings (0.62 vs 0.24 p=0.004) but less exposure to midurethral slings (1.44 vs 2.18 p=0.001) and vaginal apical support (2.21 vs 1.72 p=0.025).
Conclusions: A comprehensive picture of resident’s experience with FPMRS procedures suggest that urology residents have more experience, and overall, more comfort with performing many common FPMRS procedures without formal fellowship training. However, it is notable that Ob/Gyn residents have significantly more experience and comfort with transvaginal procedures. Additionally, there is minimal impact of a fellowship and dedicated rotation in the exposure/comfort to FPMRS procedures.
Source of Funding: None

.jpg)
.jpg)