Back
Poster, Podium & Video Sessions
Podium
PD31: Trauma/Reconstruction/Diversion: Urethral Reconstruction (including Stricture, Diverticulum) II
PD31-03: Bladder Outlet Surgeries for Men with Stress Urinary Incontinence and Neurogenic Lower Urinary Tract Dysfunction: A Multicenter Neurogenic Bladder Research Group Study
Saturday, May 14, 2022
3:50 PM – 4:00 PM
Location: Room 252
Javier Santiago*, Ann Arbor, MI, Min Soo Choo, Seoul, Korea, Republic of, Richard Mora, Evgeniy Kreydin, David A Ginsberg, Los Angeles, CA, Natalia Hernandez, Paola Bustillos, Rose Khavari, Houston, TX, Stephanie Daignault-Newton, John Stoffel, Ann Arbor, MI
- JS
Javier E. Santiago, MD
Urology Resident
University of Michigan
Podium Presenter(s)
Introduction: We evaluated the effectiveness and durability of bladder outlet procedures for treating stress urinary incontinence (SUI) in male patients with neurogenic lower urinary tract dysfunction (NLUTD).
Methods: A retrospective multi-institutional review by the Neurogenic Bladder Research Group of male patients with NLUTD who underwent urethral bulking injection (UBI), sling placement, or artificial urinary sphincter (AUS) for SUI between 2012-2020 was performed via CPT and ICD-9 codes. Men undergoing concomitant bladder reconstruction or botulinum injections (BTX) were included. The primary outcome was procedural failure, defined as return to baseline pre-operative SUI symptoms and/or needing additional surgical intervention for SUI. Time to failure were evaluated and multi-variable analysis for variables associated with failure were assessed.
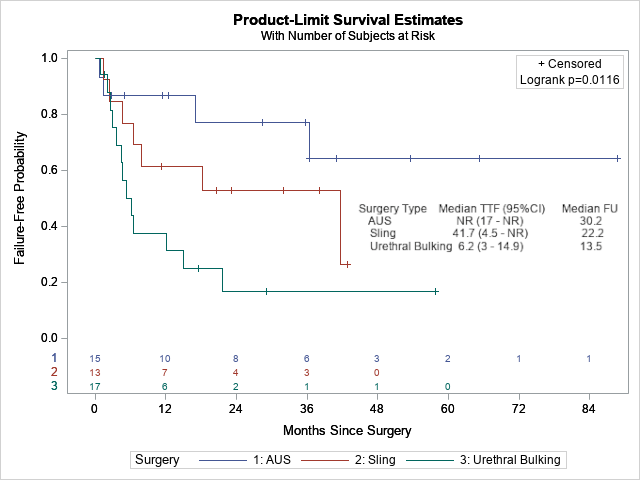
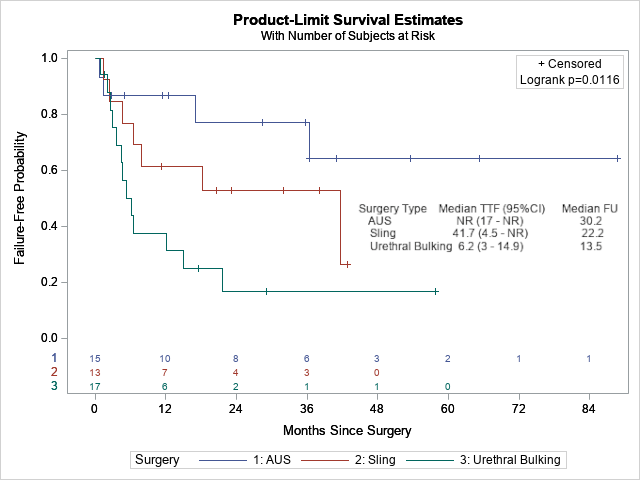
Results: Forty-five men were identified with diagnosis of spina bifida (SB) (60%), spinal cord injury (SCI) (15%), and bladder exstrophy, multiple sclerosis or auto-immune neuropathy, pelvic surgery, or a supra-pontine disorder. Bladder outlet procedures included 17, 13, and 15 cases of UBI, sling, and AUS, respectively with a median follow up of 627 days. The mean age was 33 years, and AUS had significantly older patients (mean age 50) compared to sling (20) and UBI (27) (p=0.0003). Concomitant BTX was performed exclusively with UBI (17%) and bladder reconstruction was performed more with sling vs UBI (53% vs 11%, p=0.019). AUS demonstrated the longest overall failure-free survival (Figure 1) with a failure rate of 27%, followed by sling (43%) and UBI (76%) (p=0.016). UBI was notable for rapid failure within 6 months (49.8%) compared to sling (23%) and AUS (13%). Failure was associated with increasing age, with UBI and sling compared to AUS, and SCI diagnosis (compared to SB) on multi-variable analysis.
Conclusions: Men with NLUTD and SUI had longer failure free survival with artificial urinary sphincter compared to sling and bulking agents in this multi-institutional cohort. This data can be used for counseling patients on expectations associated with bladder outlet procedures in this population.
Source of Funding: None
Methods: A retrospective multi-institutional review by the Neurogenic Bladder Research Group of male patients with NLUTD who underwent urethral bulking injection (UBI), sling placement, or artificial urinary sphincter (AUS) for SUI between 2012-2020 was performed via CPT and ICD-9 codes. Men undergoing concomitant bladder reconstruction or botulinum injections (BTX) were included. The primary outcome was procedural failure, defined as return to baseline pre-operative SUI symptoms and/or needing additional surgical intervention for SUI. Time to failure were evaluated and multi-variable analysis for variables associated with failure were assessed.
Results: Forty-five men were identified with diagnosis of spina bifida (SB) (60%), spinal cord injury (SCI) (15%), and bladder exstrophy, multiple sclerosis or auto-immune neuropathy, pelvic surgery, or a supra-pontine disorder. Bladder outlet procedures included 17, 13, and 15 cases of UBI, sling, and AUS, respectively with a median follow up of 627 days. The mean age was 33 years, and AUS had significantly older patients (mean age 50) compared to sling (20) and UBI (27) (p=0.0003). Concomitant BTX was performed exclusively with UBI (17%) and bladder reconstruction was performed more with sling vs UBI (53% vs 11%, p=0.019). AUS demonstrated the longest overall failure-free survival (Figure 1) with a failure rate of 27%, followed by sling (43%) and UBI (76%) (p=0.016). UBI was notable for rapid failure within 6 months (49.8%) compared to sling (23%) and AUS (13%). Failure was associated with increasing age, with UBI and sling compared to AUS, and SCI diagnosis (compared to SB) on multi-variable analysis.
Conclusions: Men with NLUTD and SUI had longer failure free survival with artificial urinary sphincter compared to sling and bulking agents in this multi-institutional cohort. This data can be used for counseling patients on expectations associated with bladder outlet procedures in this population.
Source of Funding: None

.jpg)
.jpg)