Back
Poster, Podium & Video Sessions
Podium
PD31: Trauma/Reconstruction/Diversion: Urethral Reconstruction (including Stricture, Diverticulum) II
PD31-05: Repeated Transurethral Interventions Increase Elastin Degradation and Stricture Severity
Saturday, May 14, 2022
4:10 PM – 4:20 PM
Location: Room 252
Michael Witthaus*, San Diego, CA, Jathin Bandari, Rochester, NY, Thomas Will Fuller, Seattle, WA, Valmik Bhargava, Jill Buckley, Mahadevan Rajasekaran, San Diego, CA
- MW
Podium Presenter(s)
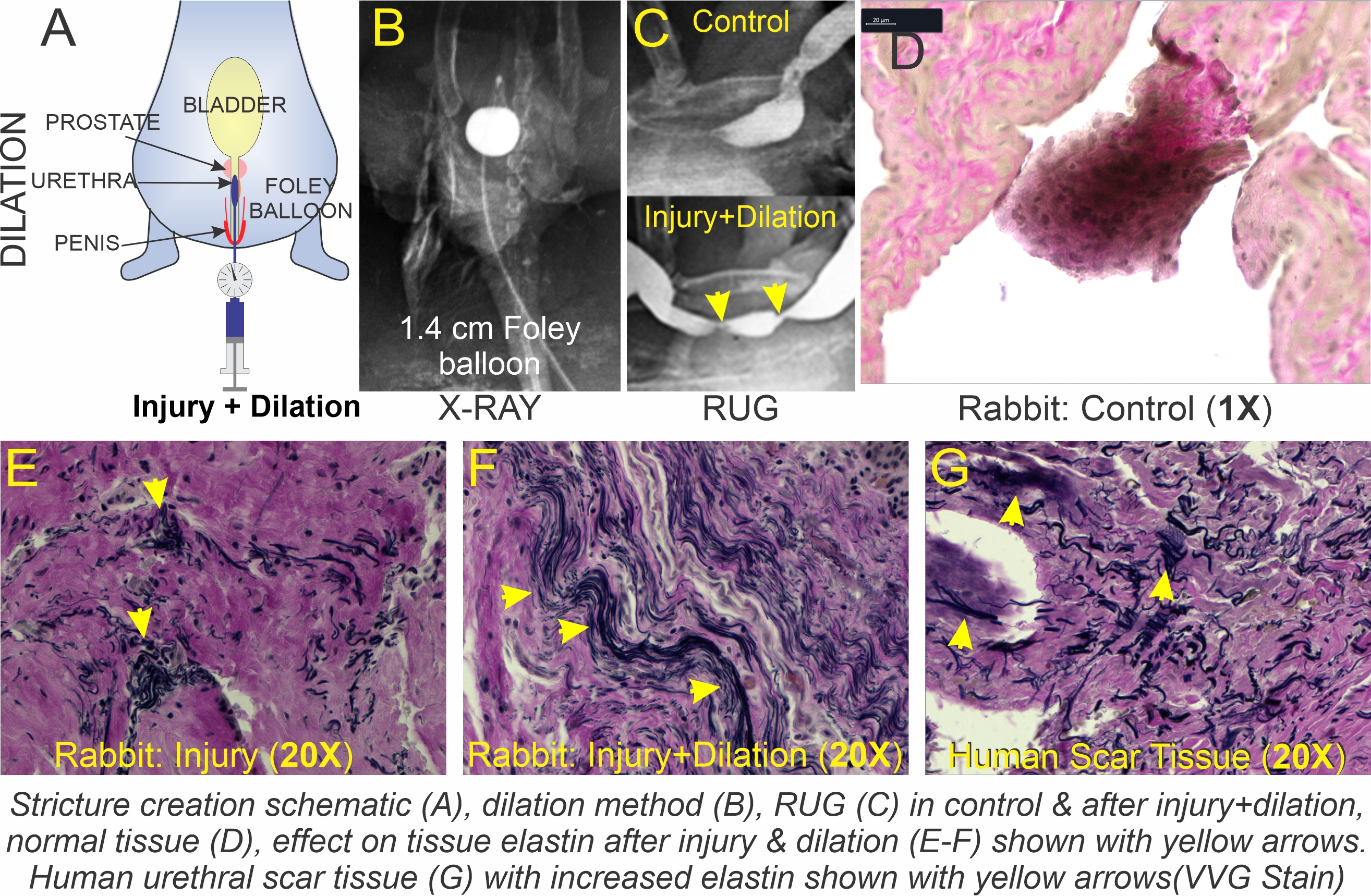
Introduction: Repeated transurethral interventions can cause or exacerbate urethral stricture disease by increasing tissue damage. A clear understanding of molecular mechanisms involved in increased fibrogenesis would enable development of optimal strategies to minimize progression or prevent stricture recurrence. Recently elastin, an extracellular matrix protein has been implicated in heart, liver and kidney fibrosis. We hypothesize repeated transurethral mechanical stretch accelerates elastin degradation and increases stricture severity.
Methods: Electrocautery was used to induce strictures in middle aged rabbits (12 months; n=6; Fig A). Rabbits (n=3) that showed evidence of stricture development at 14 days post-injury were further subjected to urethral wall stretch using a Foley catheter (balloon inflated to 14 mm diameter for 10 minutes, once a week for 4 weeks; Fig B). Animals were then allowed to recover and subjected to retrograde urethrogram (RUG) to confirm stricture progression and sacrificed at 45 days post-injury. Urethral tissues were harvested and subjected to immunostaining (Verhoeff–Van Gieson; VVG) for elastin. Results were then validated in human urethral scar tissues (n=3) obtained from patients undergoing urethroplasty.
Results: RUG findings are summarized in the Fig C. The RUGs performed showed a significant increase in stricture severity after balloon dilation (Fig C -bottom panel). The methodology utilized in the animal model was confirmed fluoroscopically to be replicable. VVG showed strong labeling for elastin (Fig E-F; black stain; yellow arrows) in rabbit and human (Fig G) scar tissues relative to controls (Fig D).
Conclusions: Our findings confirm that this approach is a viable model to study transurethral intervention induced fibrogenesis. It further supports our hypothesis that urethral wall stretch worsens stricture severity due to elastin degradation. This may be an initiating factor in tissue remodeling after injury. Targeting elastin using an elastase may be a potential pharmacological intervention to treat or prevent stricture recurrence after transurethral interventions.
Source of Funding: UCSD Academic Senate
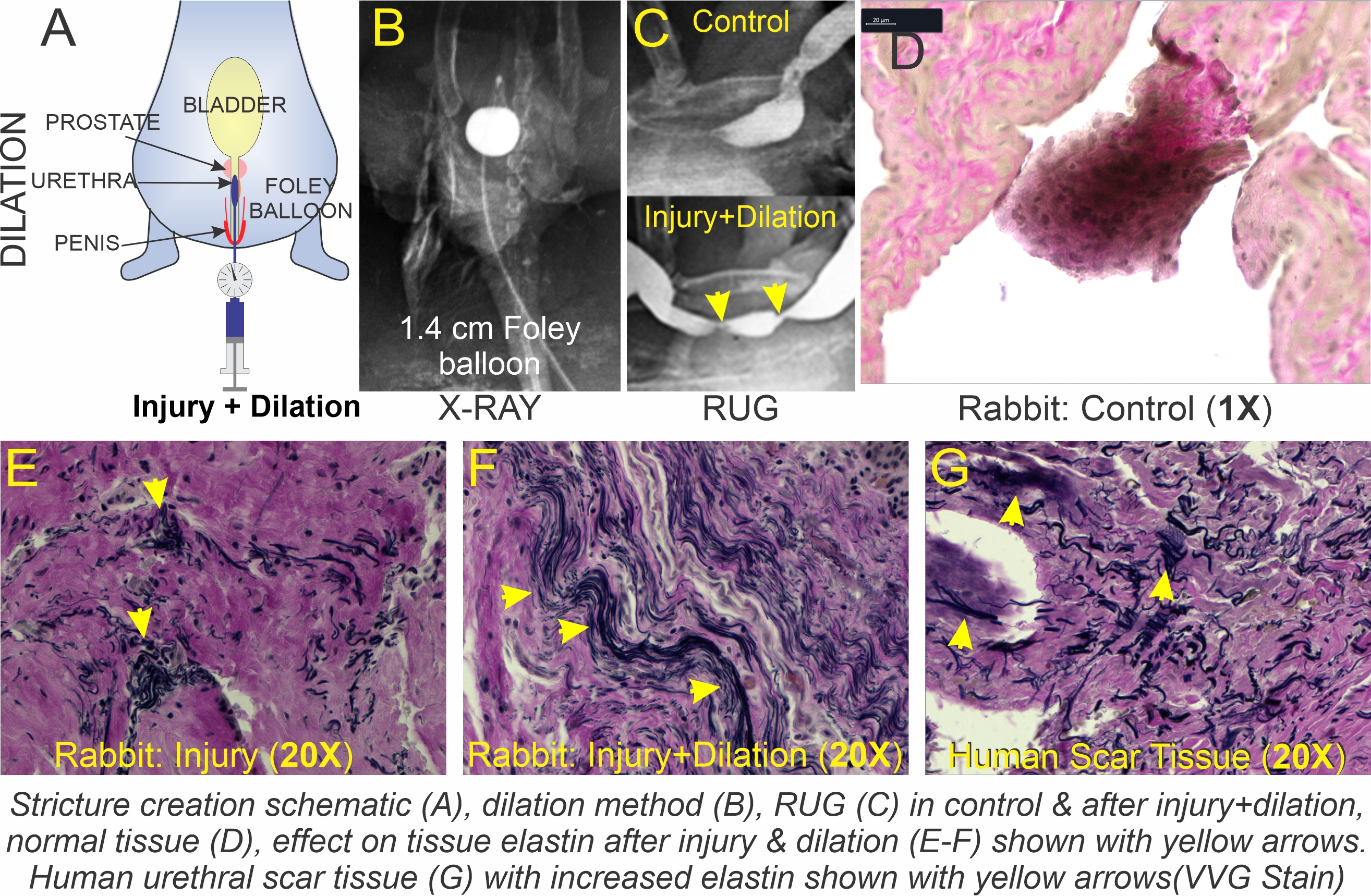
Methods: Electrocautery was used to induce strictures in middle aged rabbits (12 months; n=6; Fig A). Rabbits (n=3) that showed evidence of stricture development at 14 days post-injury were further subjected to urethral wall stretch using a Foley catheter (balloon inflated to 14 mm diameter for 10 minutes, once a week for 4 weeks; Fig B). Animals were then allowed to recover and subjected to retrograde urethrogram (RUG) to confirm stricture progression and sacrificed at 45 days post-injury. Urethral tissues were harvested and subjected to immunostaining (Verhoeff–Van Gieson; VVG) for elastin. Results were then validated in human urethral scar tissues (n=3) obtained from patients undergoing urethroplasty.
Results: RUG findings are summarized in the Fig C. The RUGs performed showed a significant increase in stricture severity after balloon dilation (Fig C -bottom panel). The methodology utilized in the animal model was confirmed fluoroscopically to be replicable. VVG showed strong labeling for elastin (Fig E-F; black stain; yellow arrows) in rabbit and human (Fig G) scar tissues relative to controls (Fig D).
Conclusions: Our findings confirm that this approach is a viable model to study transurethral intervention induced fibrogenesis. It further supports our hypothesis that urethral wall stretch worsens stricture severity due to elastin degradation. This may be an initiating factor in tissue remodeling after injury. Targeting elastin using an elastase may be a potential pharmacological intervention to treat or prevent stricture recurrence after transurethral interventions.
Source of Funding: UCSD Academic Senate

.jpg)
.jpg)