Back
Poster, Podium & Video Sessions
Podium
PD31: Trauma/Reconstruction/Diversion: Urethral Reconstruction (including Stricture, Diverticulum) II
PD31-10: Patient and Stricture Variables Associated with Failure after Urethroplasty for Bulbar Urethral Strictures
Saturday, May 14, 2022
5:00 PM – 5:10 PM
Location: Room 252
Kevin Flynn*, Iowa City, IA, Shawn Grove, Minneapolis, MN, Nejd Alsikafi, Gurnee, IL, Joshua Broghammer, Kansas City, KS, Jill Buckley, San Diego, CA, Sean Elliott, Minneapolis, MN, Jeremy Myers, Salt Lake City, UT, Andrew Peterson, Durham , NC, Keith Rourke, Edmonton , Canada, Thomas Smith III, Houston, TX, Alex Vanni, Burlington, MA, Lee Zhao, New York City, NY, Bradley Erickson, Iowa City, IA

Kevin J. Flynn, MD
Resident Physician
University of Iowa
Podium Presenter(s)
Introduction: Urethroplasty is the gold standard treatment for urethral stricture disease (USD) with historically high success rates. Still, failures occur and reasons for failure are not always readily apparent. While variations in technique (i.e. dorsal/ventral buccal placement, excisional/non-transection) may play some role, studies have yet to show clear superiority of one modern technique over another when performed by surgeons facile with a specific technique. Herein we look at patient and stricture variables, and their association with bulbar stricture urethroplasty (BU) failure, from a large multi-institutional surgical outcomes study group.
Methods: The Trauma and Urologic Reconstruction Network of Surgeons (TURNS) prospective database was used to create a cohort of bulbar (S1a/S1b; no posterior or penile urethral extension) urethral strictures that underwent single-stage BU from 2010 to 2018 with minimum 3-year clinical follow-up (database + retrospective chart review) not associated with hypospadias. Patient (BMI, age) and stricture (length, etiology, prior endoscopic procedures, location) variables were analyzed for association with failure (secondary repair and/or inability to traverse repair with flexible cystoscope) using both uni- and multivariable methods.
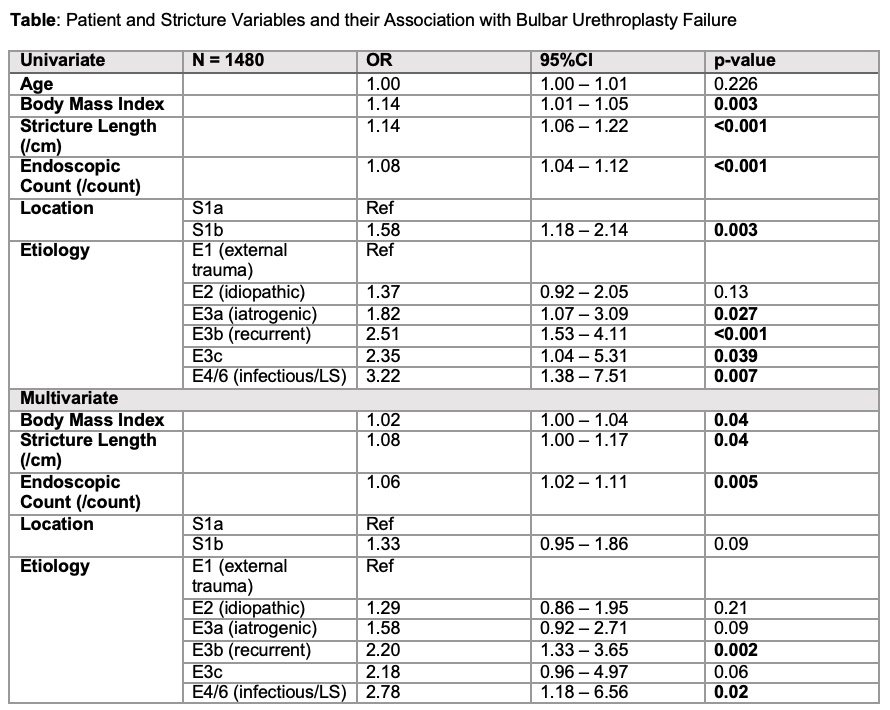
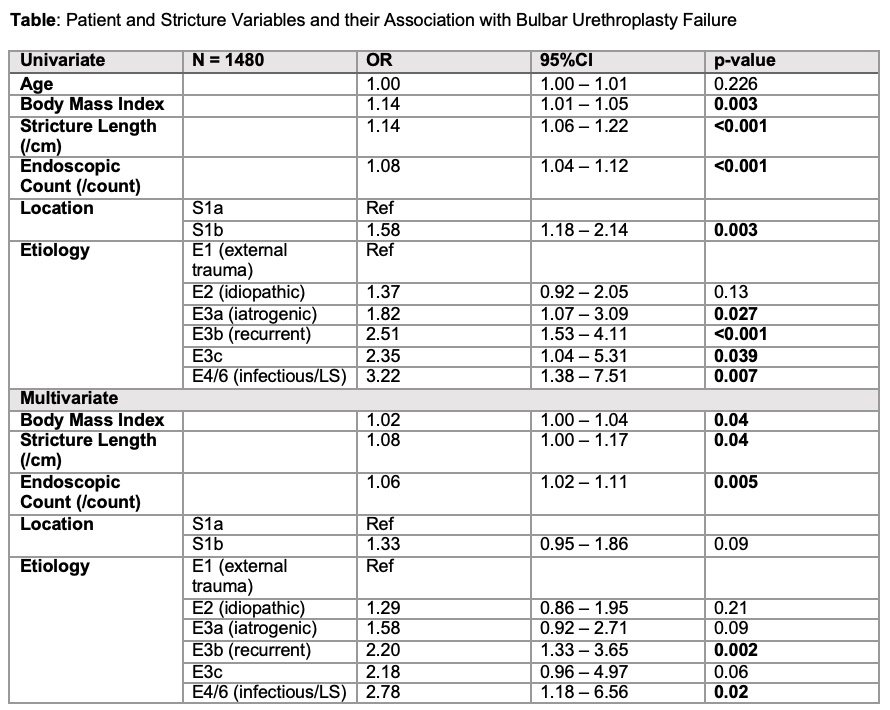
Results: At a median follow-up time was 65.1 months there were 195 (13.2%) failures amongst the 1480 patients undergoing BU. The uni- and multi-variable predictors of failure are shown in the Table. All variables other than age were associated with failure in univariable models. In the multivariable model, factors statistically associated with failure included higher BMI, pre-urethroplasty endoscopic procedure count, recurrent strictures and inflammatory strictures, with distal bulbar extension and radiation history nearing significance.
Conclusions: A multitude of readily obtainable patient and stricture variables were found to be independently associated with BU failure in this large cohort of patients with long follow-up, including stricture length, pre-urethroplasty endoscopic count, BMI and stricture etiology, validating associations previously noted in smaller cohorts.
Source of Funding: NIDDK 1R21DK115945-01
Methods: The Trauma and Urologic Reconstruction Network of Surgeons (TURNS) prospective database was used to create a cohort of bulbar (S1a/S1b; no posterior or penile urethral extension) urethral strictures that underwent single-stage BU from 2010 to 2018 with minimum 3-year clinical follow-up (database + retrospective chart review) not associated with hypospadias. Patient (BMI, age) and stricture (length, etiology, prior endoscopic procedures, location) variables were analyzed for association with failure (secondary repair and/or inability to traverse repair with flexible cystoscope) using both uni- and multivariable methods.
Results: At a median follow-up time was 65.1 months there were 195 (13.2%) failures amongst the 1480 patients undergoing BU. The uni- and multi-variable predictors of failure are shown in the Table. All variables other than age were associated with failure in univariable models. In the multivariable model, factors statistically associated with failure included higher BMI, pre-urethroplasty endoscopic procedure count, recurrent strictures and inflammatory strictures, with distal bulbar extension and radiation history nearing significance.
Conclusions: A multitude of readily obtainable patient and stricture variables were found to be independently associated with BU failure in this large cohort of patients with long follow-up, including stricture length, pre-urethroplasty endoscopic count, BMI and stricture etiology, validating associations previously noted in smaller cohorts.
Source of Funding: NIDDK 1R21DK115945-01

.jpg)
.jpg)