Back
Poster, Podium & Video Sessions
Podium
PD33: Kidney Cancer: Localized: Surgical Therapy II
PD33-10: Nephrometry and Cumulative Morbidity After Partial Nephrectomy: a Standardized Assessment of Complications in the Context of R.E.N.A.L. And PADUA Scores
Saturday, May 14, 2022
4:50 PM – 5:00 PM
Location: Room 245
Dejan K. Filipas*, Hang Yu, Clemens Spink, Michael Rink, Silke Riechardt, Philipp Gild, Phillip Marks, Margit Fisch, Roland Dahlem, Hamburg, Germany, Christian P. Meyer, Herford, Germany, Malte W. Vetterlein, Hamburg, Germany
- DF
Podium Presenter(s)
Introduction: Nephrometry scores aid in clinical decision-making and improve preoperative risk assessment in patients with renal masses scheduled for surgery. However, there is a lack of knowledge whether nephrometry scores are correlated with cumulative morbidity after partial nephrectomy (PN). We aimed to evaluate the association of PADUA and R.E.N.A.L. scores with the 30-d Comprehensive Complication Index (CCI®) after PN for renal masses.
Methods: Patients undergoing PN between 01/2019-08/2020 with preoperative imaging were included. R.E.N.A.L. and PADUA scores were calculated for each patient and 30-d complications were extracted from digital charts according to both a procedure-specific predefined catalog and the EAU Guidelines on Reporting and Grading of Complications. Pearson correlation was performed to evaluate the relationship between R.E.N.A.L/PADUA scores with the CCI®, which reflects cumulative morbidity on a scale from 0-100 and is based on the validated Clavien-Dindo classification.
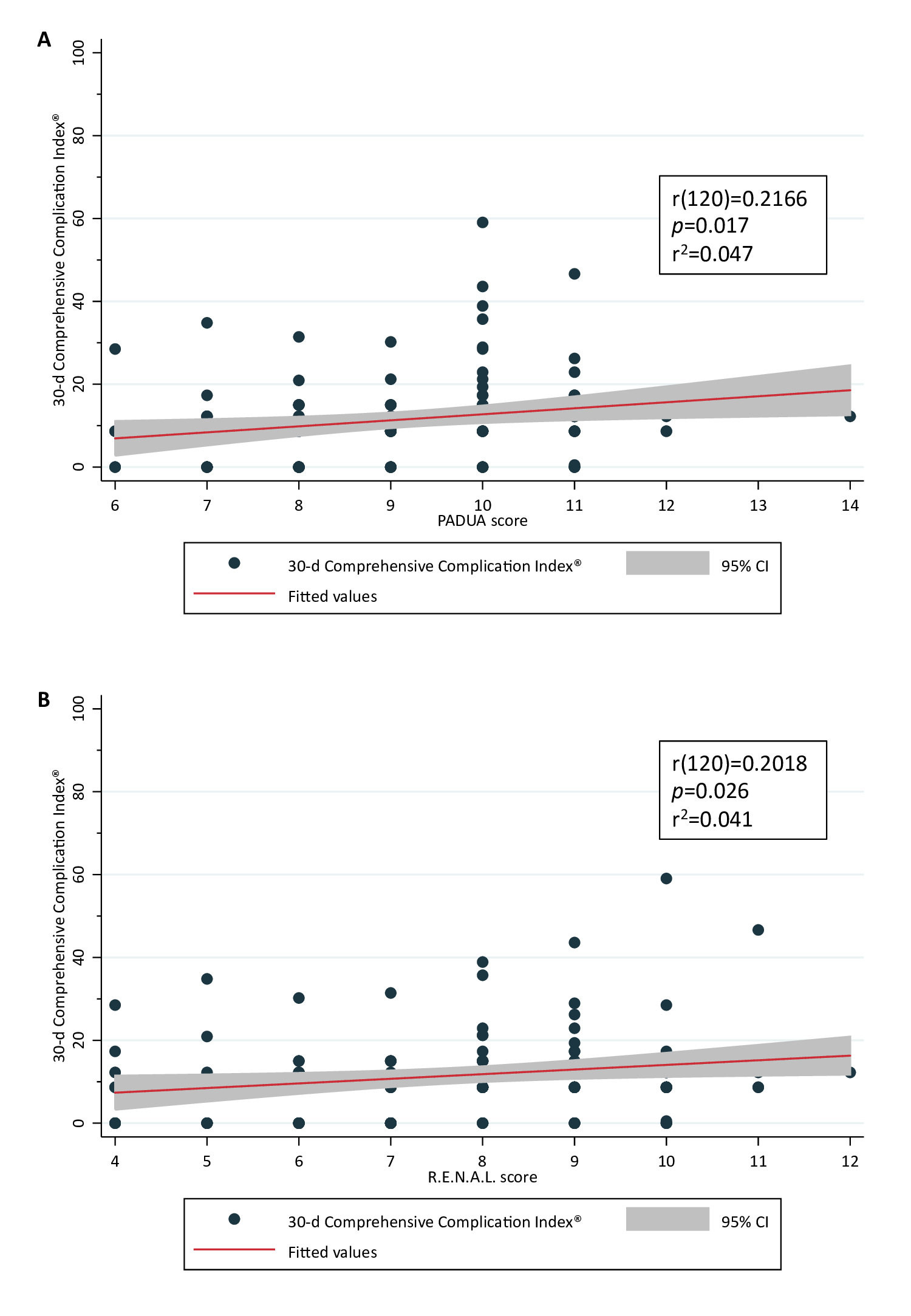
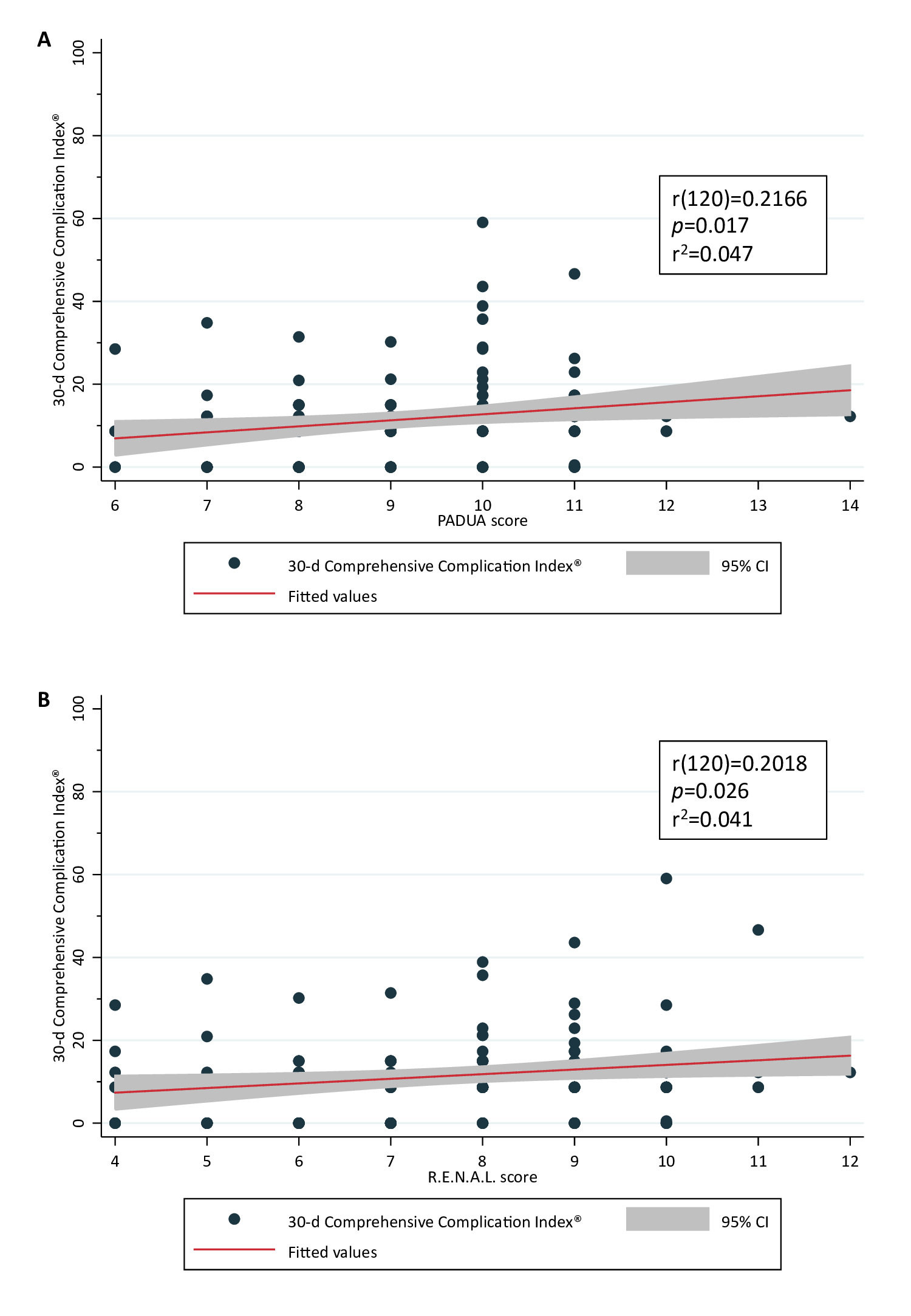
Results: Of 122 patients, 101 (83%) underwent open and 21 (17%) robot-assisted PN for renal cell carcinoma, benign lesions, or other malignancies in 85 (70%), 29 (24%), and 8 (6.6) of the cases, respectively. Median PADUA and R.E.N.A.L. scores were 9 (IQR 8-10) and 8 (IQR 6-9), respectively. Overall, 218 complications were captured in 92 patients (75%), of which 95% were classified as Clavien-Dindo =IIIa. Overall median CCI® was 8.7 (IQR 0.50-15). In PADUA low (score 6-7), moderate (score 8-9), and high complexity (score 10-14) groups there was a difference in median CCI® (8.7 vs. 8.7 vs. 12; p=0.002), which was not confirmed for R.E.N.A.L low (score 4-6), moderate (score 7-9), and high complexity (score 10-12) groups (8.7 vs. 12 vs. 10; p=0.074). There was a small positive correlation between PADUA or R.E.N.A.L. score with CCI® (Figure 1), explaining only 4.7% and 4.1% of the variation in CCI®, respectively.
Conclusions: In a tertiary referral center, PN can be safely performed with low short-term morbidity. Increasing tumor complexity as measured by validated nephrometry scores does not negatively impact perioperative complications when employing a standardized complication assessment and using the novel CCI® to capture comprehensive, cumulative morbidity.
Source of Funding: n/a
Methods: Patients undergoing PN between 01/2019-08/2020 with preoperative imaging were included. R.E.N.A.L. and PADUA scores were calculated for each patient and 30-d complications were extracted from digital charts according to both a procedure-specific predefined catalog and the EAU Guidelines on Reporting and Grading of Complications. Pearson correlation was performed to evaluate the relationship between R.E.N.A.L/PADUA scores with the CCI®, which reflects cumulative morbidity on a scale from 0-100 and is based on the validated Clavien-Dindo classification.
Results: Of 122 patients, 101 (83%) underwent open and 21 (17%) robot-assisted PN for renal cell carcinoma, benign lesions, or other malignancies in 85 (70%), 29 (24%), and 8 (6.6) of the cases, respectively. Median PADUA and R.E.N.A.L. scores were 9 (IQR 8-10) and 8 (IQR 6-9), respectively. Overall, 218 complications were captured in 92 patients (75%), of which 95% were classified as Clavien-Dindo =IIIa. Overall median CCI® was 8.7 (IQR 0.50-15). In PADUA low (score 6-7), moderate (score 8-9), and high complexity (score 10-14) groups there was a difference in median CCI® (8.7 vs. 8.7 vs. 12; p=0.002), which was not confirmed for R.E.N.A.L low (score 4-6), moderate (score 7-9), and high complexity (score 10-12) groups (8.7 vs. 12 vs. 10; p=0.074). There was a small positive correlation between PADUA or R.E.N.A.L. score with CCI® (Figure 1), explaining only 4.7% and 4.1% of the variation in CCI®, respectively.
Conclusions: In a tertiary referral center, PN can be safely performed with low short-term morbidity. Increasing tumor complexity as measured by validated nephrometry scores does not negatively impact perioperative complications when employing a standardized complication assessment and using the novel CCI® to capture comprehensive, cumulative morbidity.
Source of Funding: n/a

.jpg)
.jpg)