Back
Poster, Podium & Video Sessions
Podium
PD33: Kidney Cancer: Localized: Surgical Therapy II
PD33-12: Pre-operative risk calculator of the probability of completing nephron-sparing surgery for kidney cancer based on tumour complexity and surgical approach
Saturday, May 14, 2022
5:00 PM – 5:10 PM
Location: Room 245
Alessandro Larcher, Francesco Cei, Giuseppe Rosiello, Giacomo Musso, Giuseppe Fallara, Chiara Re, Daniele Cignoli, Giuseppe Basile*, Gianmarco Colandrea, Gianfranco Baiamonte, Isaline Rowe, Daniela Canibus, Milan, Italy, Federico Dehò, Varese, Italy, Andrea Gallina, Milan, Italy, Alexandre Mottrie, Aalst, Belgium, Cristina Giancristofaro, Francesco De Cobelli, Giorgio Brembilla, Alberto Briganti, Roberto Bertini, Francesco Montorsi, Andrea Salonia, Umberto Capitanio, Milan, Italy

Giuseppe Basile, MD
IRCCS San Raffaele Hospital
Podium Presenter(s)
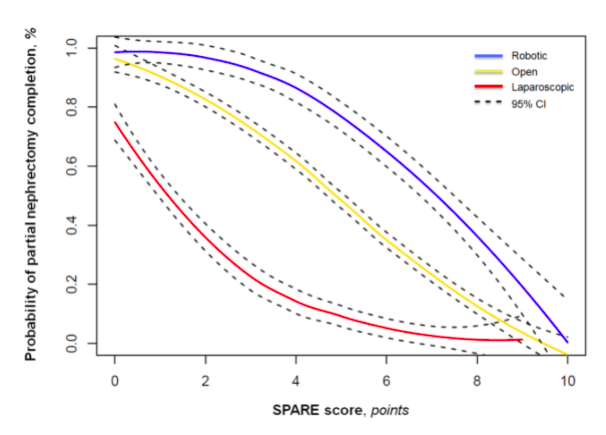
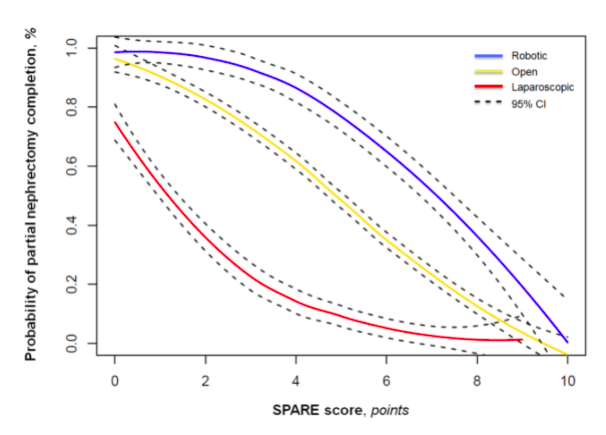
Introduction: Pre-operative estimation of the probability of completing partial (PN) relative to radical nephrectomy (RN) is invariably inaccurate. This estimation is even more complex, since the probability of completing PN might be influenced by tumour features, surgical approach (APP) and surgical experience (SE). The aim of the study is to provide for the first time a precise estimate of the probability of completing PN according to tumour complexity.
Methods: 675 patients diagnosed with a cT1-2 renal mass treated with RN or PN by 7 individual surgeons who performed overall more than 50 cases each at a single high-volume Institution were assessed in a prospective database. SPARE nephrometry score was used to evaluate tumour complexity. Multivariable logistic regression models were used to estimate the probability of completing PN. Predictors consisted of age, eGFR, clinical tumour size, SE, APP, SPARE, and ECOG PS. Since a non-linear relationship may exist between continuous variables and the outcome, restricted cubic splines were used. Finally, for clinical purposes, we built a risk calculator based on the regression coefficients.
Results: Patients treated with PN had lower median clinical tumour size (3.3 vs. 6.7), lower median SPARE score (2 vs. 7) and more favorable clinical T stage (p < 0.001) compared to RN counterparts. At logistic regression analysis predicting PN completion relative to RN, smaller clinical tumour size, open or robot-assisted relative to laparoscopic APP, higher surgical experience and lower SPARE score were significantly associated with higher probability of PN completion (all p<0.01). Conversely, pre-operative eGFR, patient’s age and ECOG PS were not associated with the probability of PN completion (all p>0.05). C-index of the model was 0.94.
Conclusions: For the first time, in patients diagnosed with a cT1-2 renal mass and elected for surgical treatment, it is possible to estimate the probability of PN completion with optimal predictive accuracy using the proposed risk calculator. This key estimation can be very useful for urologists to plan the best treatment strategy (open vs. laparoscopic vs. robotic) and for patients to be properly informed about their treatment plan.
Source of Funding: no
Methods: 675 patients diagnosed with a cT1-2 renal mass treated with RN or PN by 7 individual surgeons who performed overall more than 50 cases each at a single high-volume Institution were assessed in a prospective database. SPARE nephrometry score was used to evaluate tumour complexity. Multivariable logistic regression models were used to estimate the probability of completing PN. Predictors consisted of age, eGFR, clinical tumour size, SE, APP, SPARE, and ECOG PS. Since a non-linear relationship may exist between continuous variables and the outcome, restricted cubic splines were used. Finally, for clinical purposes, we built a risk calculator based on the regression coefficients.
Results: Patients treated with PN had lower median clinical tumour size (3.3 vs. 6.7), lower median SPARE score (2 vs. 7) and more favorable clinical T stage (p < 0.001) compared to RN counterparts. At logistic regression analysis predicting PN completion relative to RN, smaller clinical tumour size, open or robot-assisted relative to laparoscopic APP, higher surgical experience and lower SPARE score were significantly associated with higher probability of PN completion (all p<0.01). Conversely, pre-operative eGFR, patient’s age and ECOG PS were not associated with the probability of PN completion (all p>0.05). C-index of the model was 0.94.
Conclusions: For the first time, in patients diagnosed with a cT1-2 renal mass and elected for surgical treatment, it is possible to estimate the probability of PN completion with optimal predictive accuracy using the proposed risk calculator. This key estimation can be very useful for urologists to plan the best treatment strategy (open vs. laparoscopic vs. robotic) and for patients to be properly informed about their treatment plan.
Source of Funding: no

.jpg)
.jpg)