Back
Poster, Podium & Video Sessions
Podium
PD34: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Female Incontinence: Therapy II
PD34-04: Impact of Cognitive Function in Older Patients Undergoing Sacral Neuromodulation for Overactive Bladder: A Prospective Study
Saturday, May 14, 2022
4:00 PM – 4:10 PM
Location: Room 244
Jacqueline Zillioux*, Sarah Martin, Lauren Gleich, Glenn T. Werneburg, Emily Slopnick, Raymond R. Rackley, Sandip Vasavada, Bradley Gill, Howard B. Goldman, Cleveland, OH

Jacqueline Zillioux, MD
Cleveland Clinic
Podium Presenter(s)
Introduction: Overactive bladder (OAB) and cognitive impairment (CI) are both increasingly prevalent with age. Given the association between anticholinergics and dementia, there is need to optimize other therapies. SUFU/AUA OAB guidelines cite adequate cognitive function as necessary for sacral neuromodulation (SNM); however, the impact of CI on SNM in older patients remains unknown. This is an interim analysis of a prospective study assessing the impact of cognitive function on outcomes of SNM for refractory OAB.
Methods: With IRB-approval, we recruited patients aged =60 years scheduled for test-phase (peripheral nerve evaluation (PNE) or stage 1) SNM for refractory OAB. Baseline cognitive function was assessed using the validated Montreal Cognitive Assessment (MoCA) screening test. Scores =26/30 are considered normal and <26 considered CI. Patients completed validated questionnaires (OAB-q SF, IIQ7, UDI-6, PGI-I) at baseline and 1-month follow-up (if implanted). Number of program adjustments performed by the patient and whether patients demonstrated appropriate device use (i.e. familiarity with communicator/programmer) were recorded. Implant rate, patient-reported questionnaires, and SNM utilization were compared based on MoCA/CI.
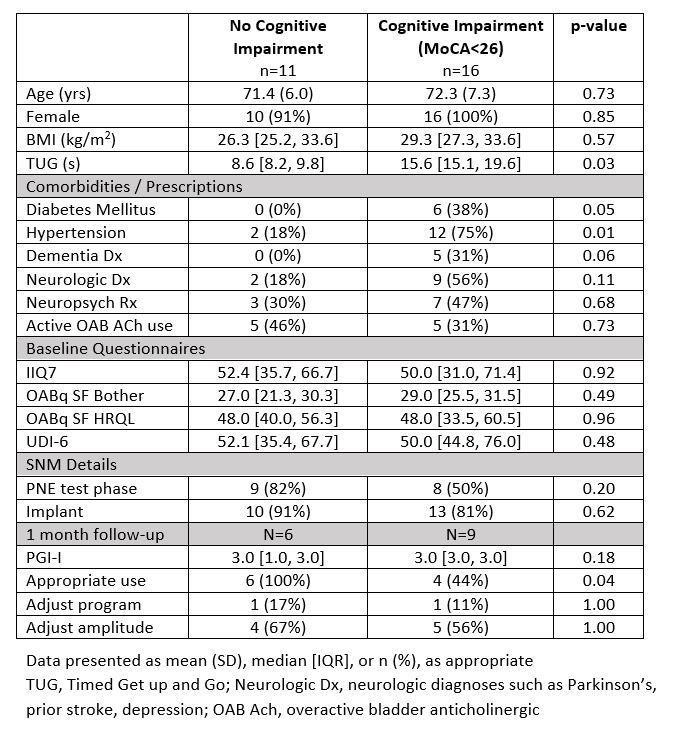
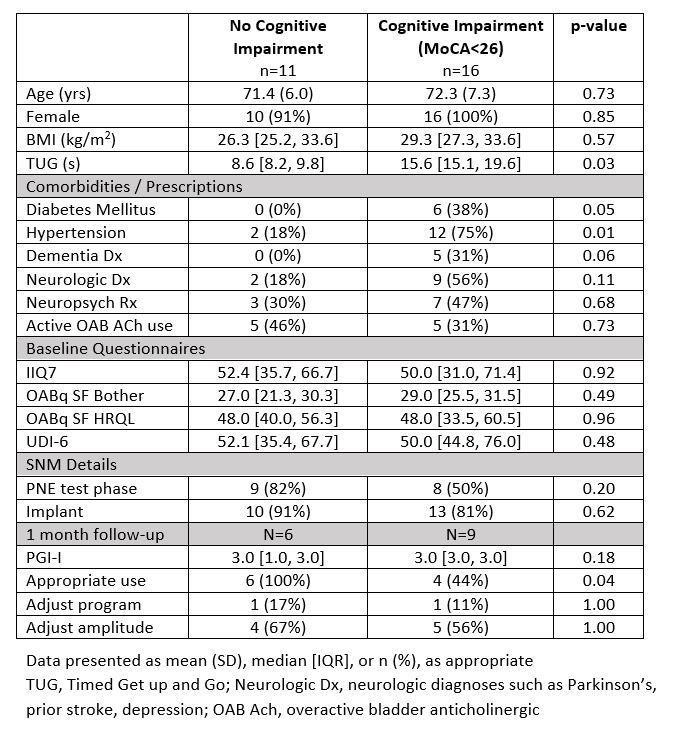
Results: 27 patients underwent test-phase (17 PNE, 10 Stage 1). Mean age was 71.9 (6.7) years. Median baseline MoCA was 24 [21.5,26.5], ranging 14-29. Although 5 (19%) patients had a pre-existing CI diagnosis, 16 (59%) demonstrated CI per MoCA. The table compares patient characteristics, baseline questionnaires and utilization outcomes based on CI. Overall, 23 (85%) patients underwent permanent implant after successful test-phase. Implant rates did not differ based on MoCA or CI. Among 15 patients with 1-month follow-up, those demonstrating appropriate device use had significantly higher MoCA scores (26 vs 17, p=0.004). Postoperative change in validated questionnaires scores, however, did not differ.
Conclusions: Despite few pre-existing diagnoses, there is a high incidence of CI in older patients with OAB undergoing SNM. While implant rate did not differ based on MoCA/CI, patients with lower MoCA scores were less likely to demonstrate appropriate device use on follow-up. Impact on clinical efficacy of SNM remains to be determined.
Source of Funding: Medtronic
Methods: With IRB-approval, we recruited patients aged =60 years scheduled for test-phase (peripheral nerve evaluation (PNE) or stage 1) SNM for refractory OAB. Baseline cognitive function was assessed using the validated Montreal Cognitive Assessment (MoCA) screening test. Scores =26/30 are considered normal and <26 considered CI. Patients completed validated questionnaires (OAB-q SF, IIQ7, UDI-6, PGI-I) at baseline and 1-month follow-up (if implanted). Number of program adjustments performed by the patient and whether patients demonstrated appropriate device use (i.e. familiarity with communicator/programmer) were recorded. Implant rate, patient-reported questionnaires, and SNM utilization were compared based on MoCA/CI.
Results: 27 patients underwent test-phase (17 PNE, 10 Stage 1). Mean age was 71.9 (6.7) years. Median baseline MoCA was 24 [21.5,26.5], ranging 14-29. Although 5 (19%) patients had a pre-existing CI diagnosis, 16 (59%) demonstrated CI per MoCA. The table compares patient characteristics, baseline questionnaires and utilization outcomes based on CI. Overall, 23 (85%) patients underwent permanent implant after successful test-phase. Implant rates did not differ based on MoCA or CI. Among 15 patients with 1-month follow-up, those demonstrating appropriate device use had significantly higher MoCA scores (26 vs 17, p=0.004). Postoperative change in validated questionnaires scores, however, did not differ.
Conclusions: Despite few pre-existing diagnoses, there is a high incidence of CI in older patients with OAB undergoing SNM. While implant rate did not differ based on MoCA/CI, patients with lower MoCA scores were less likely to demonstrate appropriate device use on follow-up. Impact on clinical efficacy of SNM remains to be determined.
Source of Funding: Medtronic

.jpg)
.jpg)