Back
Poster, Podium & Video Sessions
Podium
PD34: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Female Incontinence: Therapy II
PD34-10: Do Medicaid Patients have Access to Third Line Therapies in OAB? A State-by-State Analysis
Saturday, May 14, 2022
5:00 PM – 5:10 PM
Location: Room 244
Kelly Ieong*, Stony Brook, NY, Wai Lee, Lake Success, NY, Jason Kim, Stony Brook, NY
- KI
Kelly Ieong, BS
Stony Brook Medicine
Podium Presenter(s)
Introduction: Over 75 million Americans are currently enrolled in Medicaid, and of the beneficiaries, over 45 percent are Black or Hispanic, whereas less than 20 percent of the 62 million Medicare beneficiaries are Black or Hispanic. Studies have shown that Medicaid patients have limited access to healthcare which can lead to worse health outcomes. While third line therapies for overactive bladder (OAB) provide superior efficacy with potentially fewer side effects, there is a paucity of literature studying the barriers patient face due to health disparities. We aim to assess the state-by-state access to third line OAB therapies that Medicaid patients face.
Methods: Physician fee schedules for Medicare and Medicaid services were queried from publicly available state websites. Fee schedules were queried by CPT codes 52287, 64566, 64561 and 64590, which represent intradetrusor injection of onabotulinumtoxinA (BTX), percutaneous tibial nerve modulation (PTNM), percutaneous implantation of sacral neuromodulation (SNM) neuroelectrode and insertion of peripheral neurostimulator, respectively. Paired t-test was used to compare means between Medicare and Medicaid beneficiaries.
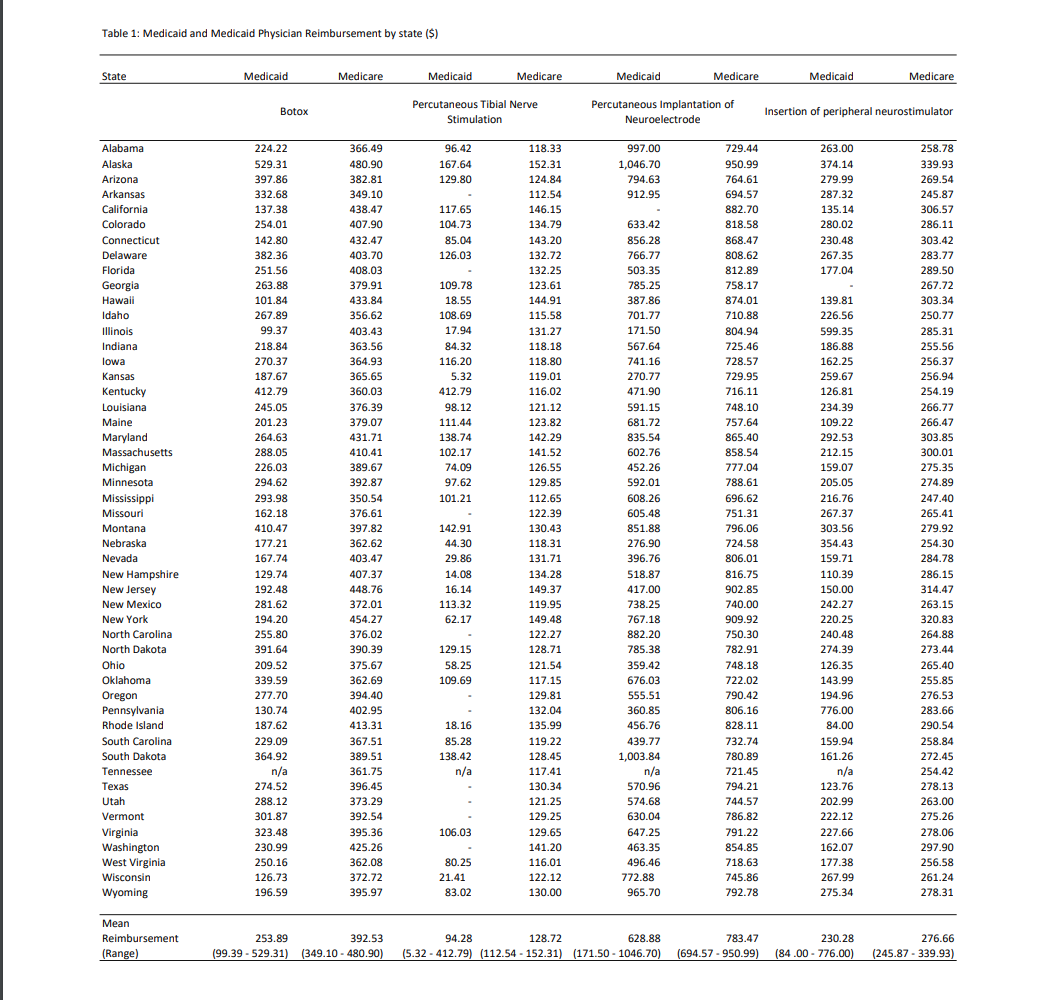
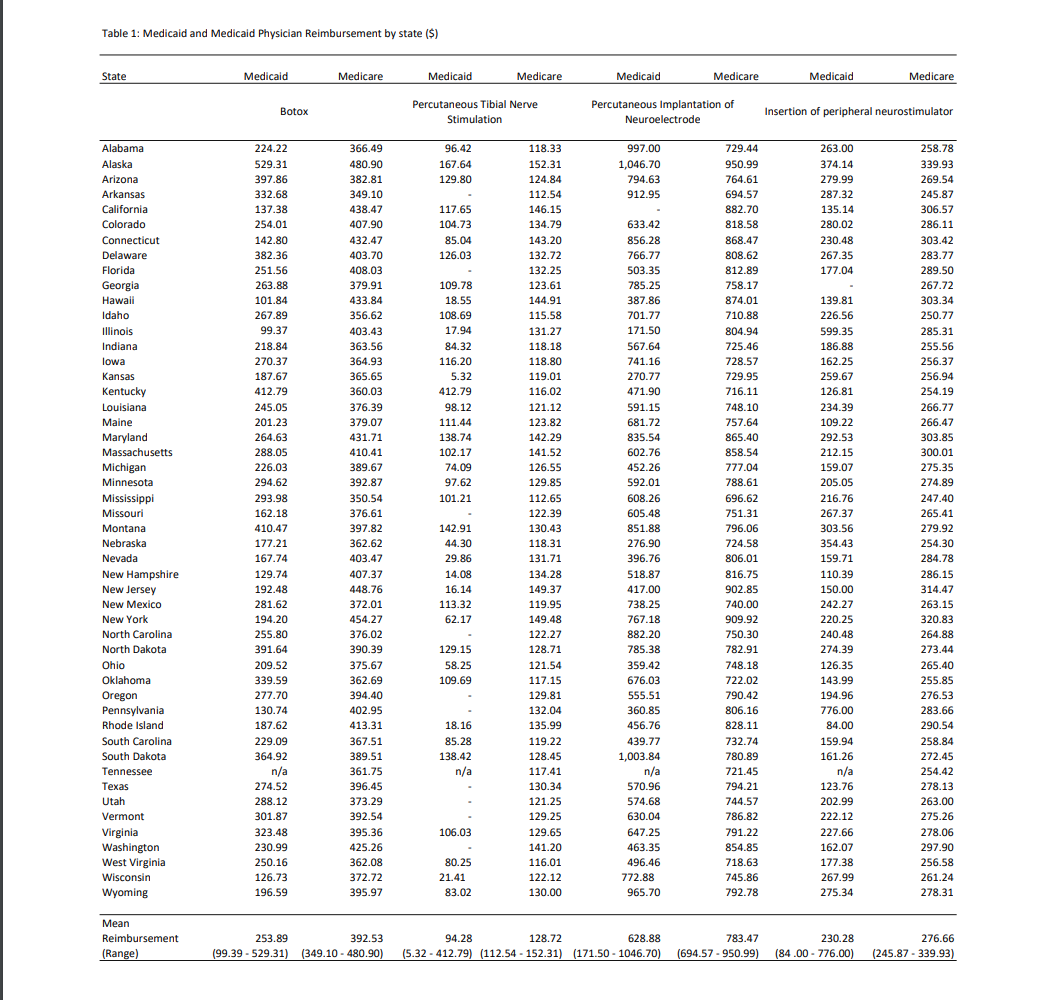
Results: Medicaid physician fee schedule was available for 49 out of 50 states. 37 states provided some form of coverage for all third line therapies. 10 states did not cover PTNM and 1 state did not cover SNM. BTX appeared to be covered in all 49 states. Medicare physician fee schedule was available for all 50 states and there was coverage in all states for all third line OAB therapies. Mean physician reimbursements were lower for Medicaid beneficiaries when compared to Medicare across all therapies. Mean physician reimbursement for BTX was $253.89 for Medicaid and $392.53 for Medicare (p < 0.001), for PTNS was $94.28 for Medicaid and $128.72 for Medicare (p=0.02), for implantation of neuroelectrode was $628.88 for Medicaid and $783.47 for Medicare (p < 0.001) and for insertion of neurostimulator was $230.28 for Medicaid and 276.66 for Medicare (p=0.005) (Table 1).
Conclusions: There is considerable variability in coverage and reimbursement rates for third line therapies amongst Medicaid beneficiaries across different states. The variability in reimbursement and coverage may have implications on access to care in this underserved patient population.
Source of Funding: none
Methods: Physician fee schedules for Medicare and Medicaid services were queried from publicly available state websites. Fee schedules were queried by CPT codes 52287, 64566, 64561 and 64590, which represent intradetrusor injection of onabotulinumtoxinA (BTX), percutaneous tibial nerve modulation (PTNM), percutaneous implantation of sacral neuromodulation (SNM) neuroelectrode and insertion of peripheral neurostimulator, respectively. Paired t-test was used to compare means between Medicare and Medicaid beneficiaries.
Results: Medicaid physician fee schedule was available for 49 out of 50 states. 37 states provided some form of coverage for all third line therapies. 10 states did not cover PTNM and 1 state did not cover SNM. BTX appeared to be covered in all 49 states. Medicare physician fee schedule was available for all 50 states and there was coverage in all states for all third line OAB therapies. Mean physician reimbursements were lower for Medicaid beneficiaries when compared to Medicare across all therapies. Mean physician reimbursement for BTX was $253.89 for Medicaid and $392.53 for Medicare (p < 0.001), for PTNS was $94.28 for Medicaid and $128.72 for Medicare (p=0.02), for implantation of neuroelectrode was $628.88 for Medicaid and $783.47 for Medicare (p < 0.001) and for insertion of neurostimulator was $230.28 for Medicaid and 276.66 for Medicare (p=0.005) (Table 1).
Conclusions: There is considerable variability in coverage and reimbursement rates for third line therapies amongst Medicaid beneficiaries across different states. The variability in reimbursement and coverage may have implications on access to care in this underserved patient population.
Source of Funding: none

.jpg)
.jpg)