Back
Poster, Podium & Video Sessions
Podium
PD35: Prostate Cancer: Advanced (including Drug Therapy) II
PD35-01: Which Patients With cN1 Disease At PET/CT Are Affected By Systemic Disease? Implications For Tailored Treatment Approaches Based On A Large Multi-Institutional Series
Sunday, May 15, 2022
7:00 AM – 7:10 AM
Location: Room 252
Elio Mazzone*, Milano, Italy, Giorgio Gandaglia, Armando Stabile, Milan, Italy, Daniele Robesti, Antony Pellegrino, Andrea Necchi, Daniele Raggi, Laura Marandino, Simone Scuderi, Francesco Barletta, Milano, Italy, Vito Cucchiara, Emanuele Zaffuto, Milan, Italy, Nazareno Suardi, Genoa, Italy, Shahrokh F. Shariat, Vienna, Austria, Francesco Montorsi, Alberto Briganti, Milano, Italy
- EM
Podium Presenter(s)
Introduction: The role of local therapies including radical prostatectomy (RP) in prostate cancer (PCa) patients with clinical lymphadenopathies at PET/CT has been scarcely explored. Limited data is available to identify men more likely to have non-localized disease and who may benefit from multi-modal approaches. We assessed predictors of PSA persistence in surgically managed PCa patients with clinical lymphadenopathies at PET/CT by integrating clinical, magnetic resonance imaging (MRI) and PET/CT parameters.
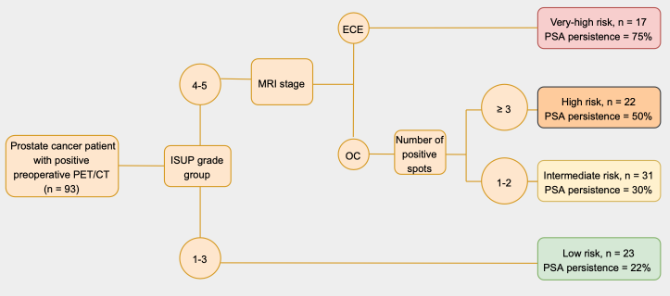
Methods: We identified 93 men treated with RP and extended lymph node dissection with pelvic or retroperitoneal lymphadenopathies at choline (n = 46, 49%) or PSMA (n = 47, 51%) PET/CT between 2010 and 2021 at four referral centers. The study outcome was PSA persistence, defined as a first PSA = 0.1 ng/ml after RP. Multivariable logistic regression tested predictors of PSA persistence. Covariates were biopsy ISUP grade group (1-3 vs 4-5), MRI stage (organ-confined disease [OC] vs extracapsular extension [ECE]) and number of positive spots at PET/CT. Regression tree analyses stratified patients into risk groups based on their preoperative characteristics.
Results: Median number of positive spots at PET/CT was 2 (IQR 1-3). Overall, 70 (75%) and 23 (25%) men had biopsy ISUP grade 4-5 and ECE at MRI. 42 (45%) experienced PSA persistence. At multivariable analyses, ISUP grade 4-5 was the strongest predictor of PSA persistence (OR 4.12; p=0.001). At regression tree, patients were stratified in four risk group according to ISUP grade, number of positive spots and MRI stage (Fig. 1). The model had a good discrimination (AUC 77%). Clinical N1 patients with ISUP grade 4-5 and ECE at MRI had a rate of 75% of PSA persistence regardless of the number of positive spots at PET/CT, thus being likely have upfront systemic disease.
Conclusions: PSA persistence is non-negligible in patients with a positive lymphnodes at preoperative PET/CT. Patients with ISUP grade 1-3, as well as patients with ISUP grade 4-5, OC disease at MRI and 1-2 positive spots at PET/CT are those where RP may achieve good oncological outcomes. Conversely, patients with high ISUP grade and ECE at MRI should be considered for integrated multi-modal approaches including systemic therapies.
Source of Funding: None.
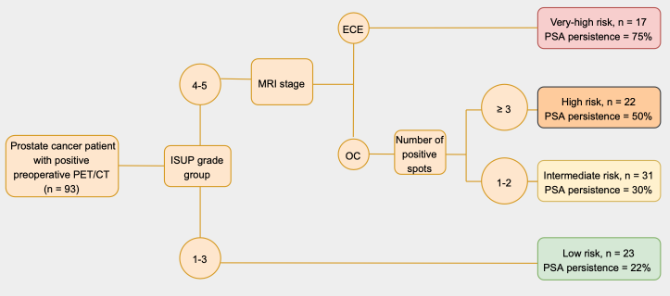
Methods: We identified 93 men treated with RP and extended lymph node dissection with pelvic or retroperitoneal lymphadenopathies at choline (n = 46, 49%) or PSMA (n = 47, 51%) PET/CT between 2010 and 2021 at four referral centers. The study outcome was PSA persistence, defined as a first PSA = 0.1 ng/ml after RP. Multivariable logistic regression tested predictors of PSA persistence. Covariates were biopsy ISUP grade group (1-3 vs 4-5), MRI stage (organ-confined disease [OC] vs extracapsular extension [ECE]) and number of positive spots at PET/CT. Regression tree analyses stratified patients into risk groups based on their preoperative characteristics.
Results: Median number of positive spots at PET/CT was 2 (IQR 1-3). Overall, 70 (75%) and 23 (25%) men had biopsy ISUP grade 4-5 and ECE at MRI. 42 (45%) experienced PSA persistence. At multivariable analyses, ISUP grade 4-5 was the strongest predictor of PSA persistence (OR 4.12; p=0.001). At regression tree, patients were stratified in four risk group according to ISUP grade, number of positive spots and MRI stage (Fig. 1). The model had a good discrimination (AUC 77%). Clinical N1 patients with ISUP grade 4-5 and ECE at MRI had a rate of 75% of PSA persistence regardless of the number of positive spots at PET/CT, thus being likely have upfront systemic disease.
Conclusions: PSA persistence is non-negligible in patients with a positive lymphnodes at preoperative PET/CT. Patients with ISUP grade 1-3, as well as patients with ISUP grade 4-5, OC disease at MRI and 1-2 positive spots at PET/CT are those where RP may achieve good oncological outcomes. Conversely, patients with high ISUP grade and ECE at MRI should be considered for integrated multi-modal approaches including systemic therapies.
Source of Funding: None.

.jpg)
.jpg)