Back
Poster, Podium & Video Sessions
Podium
PD35: Prostate Cancer: Advanced (including Drug Therapy) II
PD35-06: Health-related quality of life in low-income men after surgical castration for metastatic prostate cancer
Sunday, May 15, 2022
7:50 AM – 8:00 AM
Location: Room 252
Thomas Gaither*, Mark Litwin, Los Angeles, CA
- TG
Podium Presenter(s)
Introduction: Surgical castration for metastatic prostate cancer remains a viable treatment option, is cost-effective, and requires less follow-up. We compared outcomes in men undergoing surgical or medical castration.
Methods: We analyzed data from a prospective cohort of men enrolled in the Improving Access Counseling and Treatment for Californians with Prostate Cancer (IMPACT) program, which provides care for prostate cancer patients whose income is <200% of the federal poverty level. Outcome measures included the RAND SF-12 and the UCLA Prostate Cancer Index (PCI) at baseline and every 6 months. We used generalized estimating equations to assess the independent impact of surgical vs medical castration on quality of life.
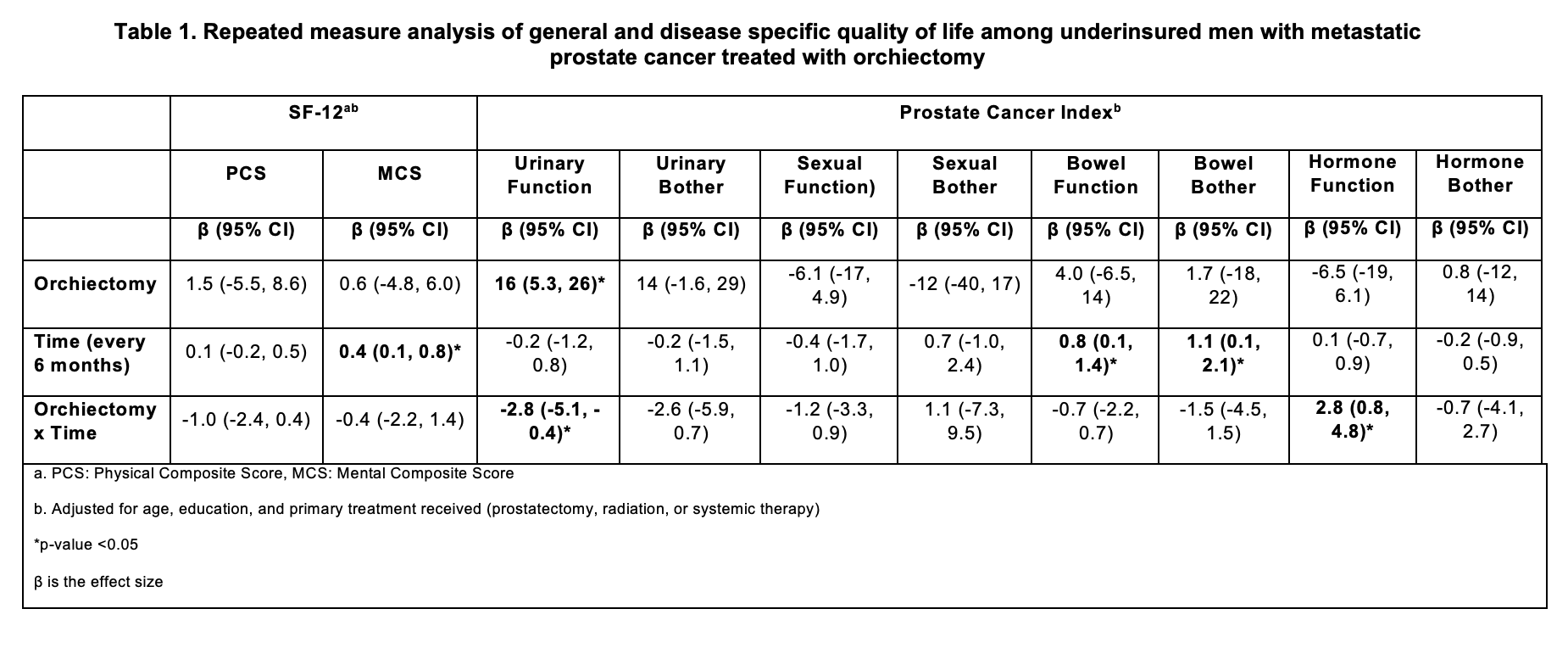
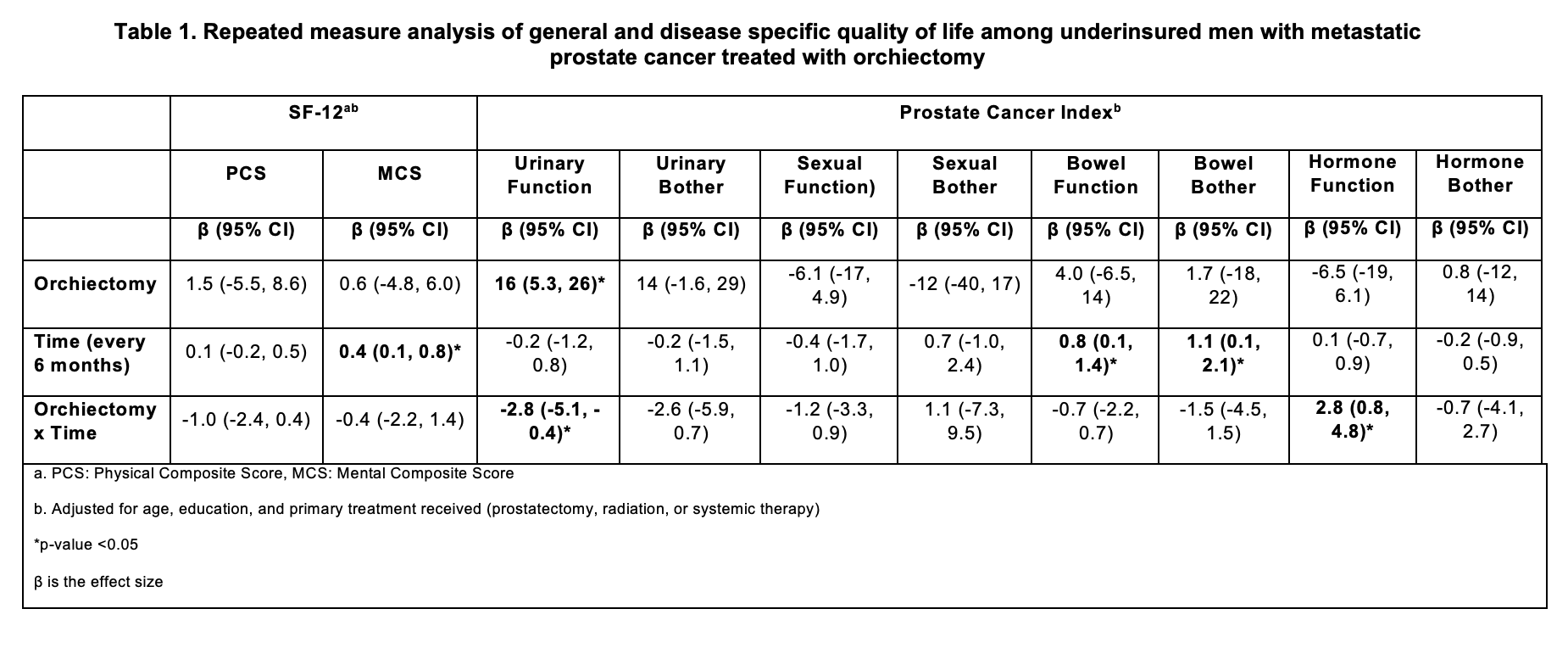
Results: Among men with metastatic prostate cancer, 27 underwent orchiectomy, and 274 underwent medical castration. Median cohort age was 61.3 years (IQR 56-65); 239 (79%) men had less than a high school education. Average follow-up was 8 months (range 0-45). The majority (66%) had metastatic disease at diagnosis. The two groups did not differ in age, race/ethnicity, education, monthly income, baseline PSA, Gleason score, or percent metastatic at diagnosis. SF-12 domains did not differ between those who underwent surgical vs medical castration (Table 1). Patients treated with orchiectomy reported better urinary function than those who underwent medical castration (+16 points, 95%CI 5.3-26). Regardless of orchiectomy status, SF-12 mental composite scores and PCI bowel function and bother scores improved over time.
Conclusions: In this large cohort of low-income, uninsured men with metastatic prostate cancer, surgical castration did not negatively impact general or disease-specific quality of life. The finding of improved urination after orchiectomy merits further inquiry. Men with castration-sensitive metastatic prostate cancer may be counseled that surgical castration is a viable option.
Source of Funding: Departmental
Methods: We analyzed data from a prospective cohort of men enrolled in the Improving Access Counseling and Treatment for Californians with Prostate Cancer (IMPACT) program, which provides care for prostate cancer patients whose income is <200% of the federal poverty level. Outcome measures included the RAND SF-12 and the UCLA Prostate Cancer Index (PCI) at baseline and every 6 months. We used generalized estimating equations to assess the independent impact of surgical vs medical castration on quality of life.
Results: Among men with metastatic prostate cancer, 27 underwent orchiectomy, and 274 underwent medical castration. Median cohort age was 61.3 years (IQR 56-65); 239 (79%) men had less than a high school education. Average follow-up was 8 months (range 0-45). The majority (66%) had metastatic disease at diagnosis. The two groups did not differ in age, race/ethnicity, education, monthly income, baseline PSA, Gleason score, or percent metastatic at diagnosis. SF-12 domains did not differ between those who underwent surgical vs medical castration (Table 1). Patients treated with orchiectomy reported better urinary function than those who underwent medical castration (+16 points, 95%CI 5.3-26). Regardless of orchiectomy status, SF-12 mental composite scores and PCI bowel function and bother scores improved over time.
Conclusions: In this large cohort of low-income, uninsured men with metastatic prostate cancer, surgical castration did not negatively impact general or disease-specific quality of life. The finding of improved urination after orchiectomy merits further inquiry. Men with castration-sensitive metastatic prostate cancer may be counseled that surgical castration is a viable option.
Source of Funding: Departmental

.jpg)
.jpg)