Back
Poster, Podium & Video Sessions
Podium
PD38: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Non-neurogenic Voiding Dysfunction II
PD38-04: A community-based education program for overactive bladder in a predominantly minority older female population: a pilot study
Sunday, May 15, 2022
7:30 AM – 7:40 AM
Location: Room 244
Susana Martinez Diaz*, Hudson Pierce, John Lee, Tirsit Asfaw, Andrew Abram, New York, NY, Naeem Bhojani, Montreal, Canada, Dean Elterman, Toronto, Canada, Kevin Zorn, Montreal, Canada, Bilal Chughtai, New York, NY
- SM
Podium Presenter(s)
Introduction: Knowledge gaps in available treatment and social stigmatization are barriers to care in patients with overactive bladder (OAB), especially for minority populations. We assess the feasibility of an OAB education program targeting older, minority community-dwelling females.
Methods: Women over age 55 were recruited from community centers in New York City. Individuals with a previous diagnosis of OAB were excluded to control for baseline knowledge about OAB. Eligible participants underwent an education program consisting of a slide presentation covering the following topics: bladder function, lower urinary tract anatomy, pathophysiology of OAB, effect of OAB on quality of life, pelvic floor exercise training, and bladder training. OAB symptom score and general and condition-specific quality of life scores were measured at baseline and 1 week, 3 months, and 6 months post-intervention using the Overactive Bladder Questionnaire-Short Form and Short Form-12. Change in scores over time was analyzed using a linear mixed-effects model for repeated measures.
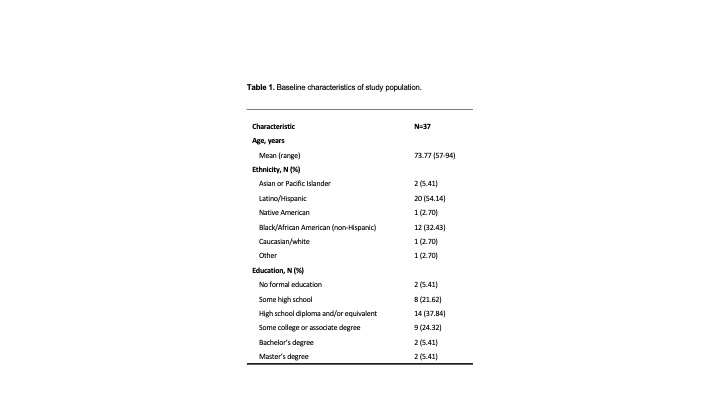
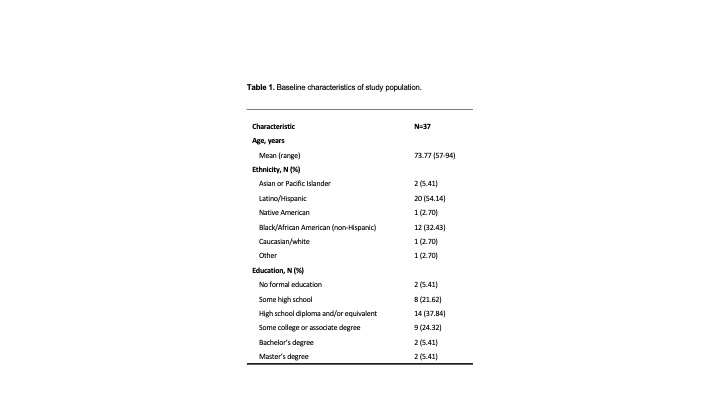
Results: 37 female patients with OAB symptoms at baseline participated in the study. Most participants were from a Latino/Hispanic or Black/African American ethnic/racial background (Table 1). For our youngest subgroup (= 68 years old) significant improvements were observed at 3 and 6 months compared to 1 week post-intervention for symptom bother (3 months, -22.75, p=0.006; 6 months, -25.76; p=0.001) and condition-specific related quality of life sub-scale scores for concern (3 months, +23.76, p=0.006; 6 months, +22.15, p=0.011) and social interaction (3 months, +21.11, p=0.017; 6 months, +20.51; p=0.021). For all ages, improvements in general quality of life measures for mental health were seen at 3 and 6 months compared to baseline (3 months, +7.57, p=0.02; 6 months, +6.70; p=0.048).
Conclusions: There were statistically significant improvements in symptom bother, condition-specific, and general quality of life measures following an OAB education program in a predominantly minority older female population. Further studies are needed to support efficacy and optimize design to benefit these patients in the long-term.
Source of Funding: Weill Cornell Clinical and Translational Science Center grant support (CTSC GRANT UL1 TR000457).
Methods: Women over age 55 were recruited from community centers in New York City. Individuals with a previous diagnosis of OAB were excluded to control for baseline knowledge about OAB. Eligible participants underwent an education program consisting of a slide presentation covering the following topics: bladder function, lower urinary tract anatomy, pathophysiology of OAB, effect of OAB on quality of life, pelvic floor exercise training, and bladder training. OAB symptom score and general and condition-specific quality of life scores were measured at baseline and 1 week, 3 months, and 6 months post-intervention using the Overactive Bladder Questionnaire-Short Form and Short Form-12. Change in scores over time was analyzed using a linear mixed-effects model for repeated measures.
Results: 37 female patients with OAB symptoms at baseline participated in the study. Most participants were from a Latino/Hispanic or Black/African American ethnic/racial background (Table 1). For our youngest subgroup (= 68 years old) significant improvements were observed at 3 and 6 months compared to 1 week post-intervention for symptom bother (3 months, -22.75, p=0.006; 6 months, -25.76; p=0.001) and condition-specific related quality of life sub-scale scores for concern (3 months, +23.76, p=0.006; 6 months, +22.15, p=0.011) and social interaction (3 months, +21.11, p=0.017; 6 months, +20.51; p=0.021). For all ages, improvements in general quality of life measures for mental health were seen at 3 and 6 months compared to baseline (3 months, +7.57, p=0.02; 6 months, +6.70; p=0.048).
Conclusions: There were statistically significant improvements in symptom bother, condition-specific, and general quality of life measures following an OAB education program in a predominantly minority older female population. Further studies are needed to support efficacy and optimize design to benefit these patients in the long-term.
Source of Funding: Weill Cornell Clinical and Translational Science Center grant support (CTSC GRANT UL1 TR000457).

.jpg)
.jpg)