Back
Poster, Podium & Video Sessions
Podium
PD39: Benign Prostatic Hyperplasia: Epidemiology, Evaluation & Medical Non-surgical Therapy
PD39-02: Does Race Influence the Surgical Treatment for Benign Prostatic Hyperplasia? - An Analysis of 30,000 Medicare Lives
Sunday, May 15, 2022
7:10 AM – 7:20 AM
Location: Room 243
Gopal L. Narang*, Scottsdale, AZ, Sirikan Rojanasarot, Michael Murphy, Ben Cutone, Marlborough, MA, Mitchell R. Humphreys, Scottsdale, AZ
- GN
Gopal Narang, MD
Mayo Clinic Arizona
Podium Presenter(s)
Introduction: The prevalence of benign prostatic hyperplasia (BPH) is increasing globally. With a greater disease burden, effective but also equitable treatment is a priority. There is little data evaluating treatment disparities for patients with BPH, specifically when considering race. This study examines the association between race and rates of BPH surgical treatment among Medicare beneficiaries.
Methods: This real-world data analysis used 5% Medicare claims data to identify newly diagnosed men with BPH, age 66, between January 2010 and December 2018. Patients were followed until either their first BPH surgery, a diagnosis of prostate or bladder cancer, end of continuous Medicare enrollment, death, or end of the study period. Cox proportional hazards regression compared the likelihood of BPH surgery between men of different races, White vs. Black, Indigenous and People of Color (BIPOC), controlling for patients’ geographical region, Charlson Comorbidity Score, and baseline comorbidities.
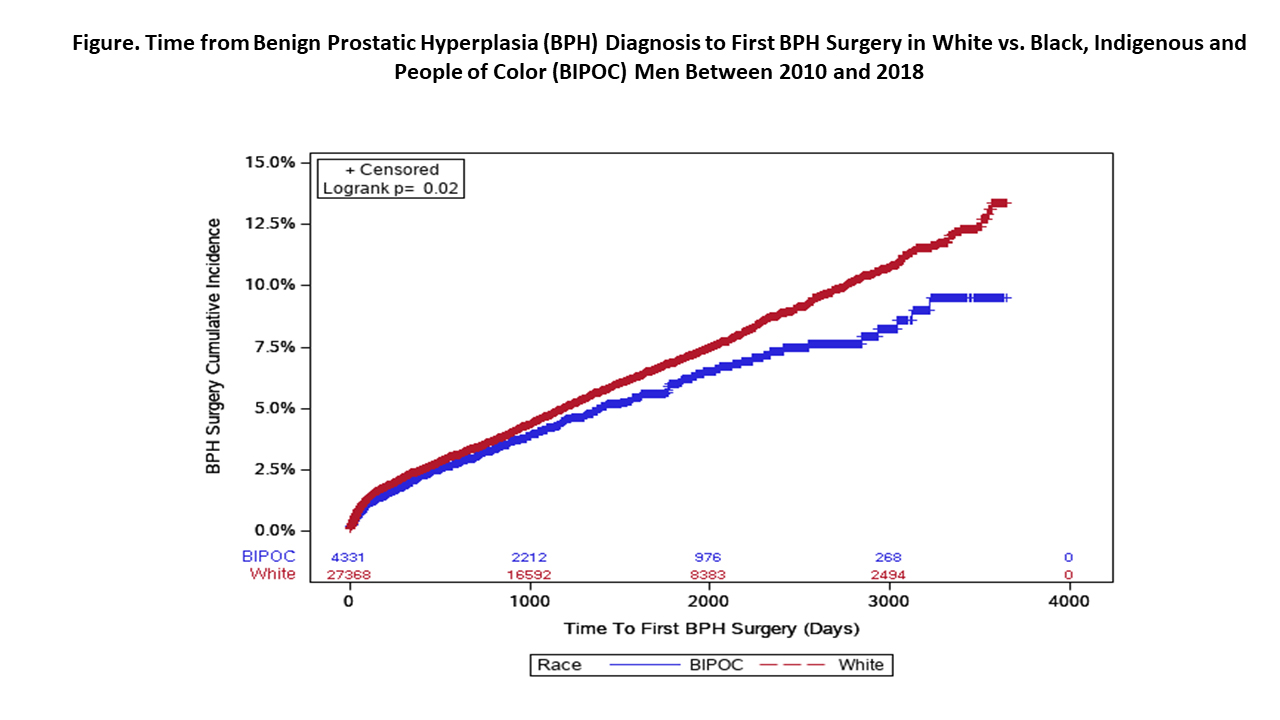
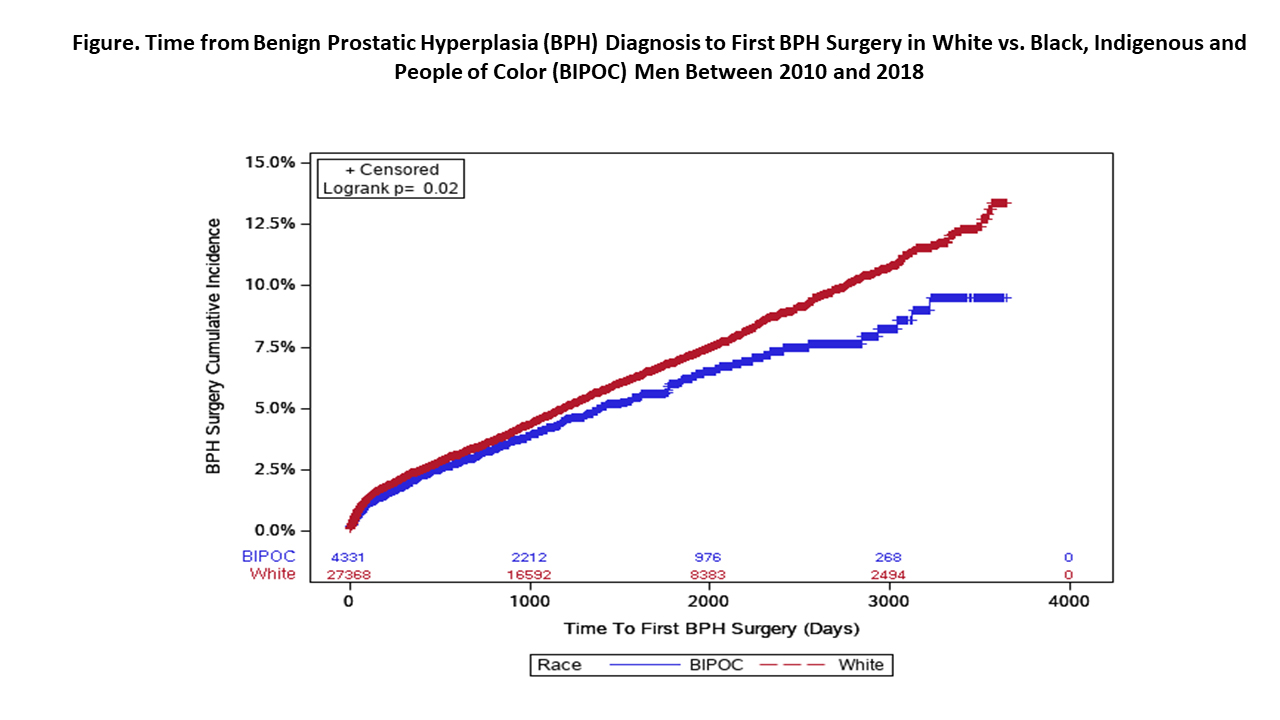
Results: The study included 31,699 men with BPH; 13.7% were BIPOC. The median follow-up was 3.6 years (IQR 1.7-6.0) for White men and 2.8 years (IQR 1.3-5.2) for BIPOC men. At the end of the study period, BIPOC men had significantly lower BPH surgery rates than White patients (9.5% vs. 13.4%, respectively; p=0.02). In multivariable-adjusted Cox regression, BIPOC race was associated with a 19% lower likelihood of receiving BPH surgery than White race (HR, 0.81; 95%CI 0.70, 0.94). Among those who had surgery, transurethral resection of the prostate was the most common surgery for both White and BIPOC groups (49.4% vs. 56.8%, respectively; p=0.05). A higher proportion of BIPOC men underwent procedures in inpatient settings compared to White men (18.2% vs. 9.8%; p=0.00).
Conclusions: Among a cohort of Medicare beneficiaries with BPH, there are notable treatment disparities when considering race. BIPOC men had lower rates of surgical treatment than White men with no difference in the type of procedure performed. BIPOC men were more likely to undergo procedures in inpatient settings. Improving patient access to BPH surgical procedures that can be performed in an outpatient setting may help address treatment disparities. Future research investigating treatment barriers and implications of site of service on access to care are needed.
Source of Funding: Boston Scientific
Methods: This real-world data analysis used 5% Medicare claims data to identify newly diagnosed men with BPH, age 66, between January 2010 and December 2018. Patients were followed until either their first BPH surgery, a diagnosis of prostate or bladder cancer, end of continuous Medicare enrollment, death, or end of the study period. Cox proportional hazards regression compared the likelihood of BPH surgery between men of different races, White vs. Black, Indigenous and People of Color (BIPOC), controlling for patients’ geographical region, Charlson Comorbidity Score, and baseline comorbidities.
Results: The study included 31,699 men with BPH; 13.7% were BIPOC. The median follow-up was 3.6 years (IQR 1.7-6.0) for White men and 2.8 years (IQR 1.3-5.2) for BIPOC men. At the end of the study period, BIPOC men had significantly lower BPH surgery rates than White patients (9.5% vs. 13.4%, respectively; p=0.02). In multivariable-adjusted Cox regression, BIPOC race was associated with a 19% lower likelihood of receiving BPH surgery than White race (HR, 0.81; 95%CI 0.70, 0.94). Among those who had surgery, transurethral resection of the prostate was the most common surgery for both White and BIPOC groups (49.4% vs. 56.8%, respectively; p=0.05). A higher proportion of BIPOC men underwent procedures in inpatient settings compared to White men (18.2% vs. 9.8%; p=0.00).
Conclusions: Among a cohort of Medicare beneficiaries with BPH, there are notable treatment disparities when considering race. BIPOC men had lower rates of surgical treatment than White men with no difference in the type of procedure performed. BIPOC men were more likely to undergo procedures in inpatient settings. Improving patient access to BPH surgical procedures that can be performed in an outpatient setting may help address treatment disparities. Future research investigating treatment barriers and implications of site of service on access to care are needed.
Source of Funding: Boston Scientific

.jpg)
.jpg)