Back
Poster, Podium & Video Sessions
Podium
PD39: Benign Prostatic Hyperplasia: Epidemiology, Evaluation & Medical Non-surgical Therapy
PD39-03: Post-voided residual urine ratio is a predictor of bladder outlet obstruction in men with lower urinary tract symptoms: development of a clinical nomogram
Sunday, May 15, 2022
7:20 AM – 7:30 AM
Location: Room 243
Cosimo De Nunzio*, Riccardo Lombardo, Rome, Italy, Antonio Nacchia, Rionero in Vulture, Italy, Antonio Cicione, Beatrice Turchi, Giacomo Gallo, Carmen Gravina, Alessandro Guercio, Jordi Stira, Lorenzo Maria Rivesti, Antonio Franco, Giorgio Guarnotta, Elisa Mancini, Olivia Alessandra Voglino, Valeria Baldassarri, Simone D'Annunzio, Sara Riolo, Rome, Italy, Simon Carter, London, United Kingdom, Carlo Vicentini, L'Aquila, Italy, Andrea Tubaro, Rome, Italy

Cosimo De Nunzio, MD,PhD
Department of Urology, Ospedale Sant'andrea, Sapienza University
Podium Presenter(s)
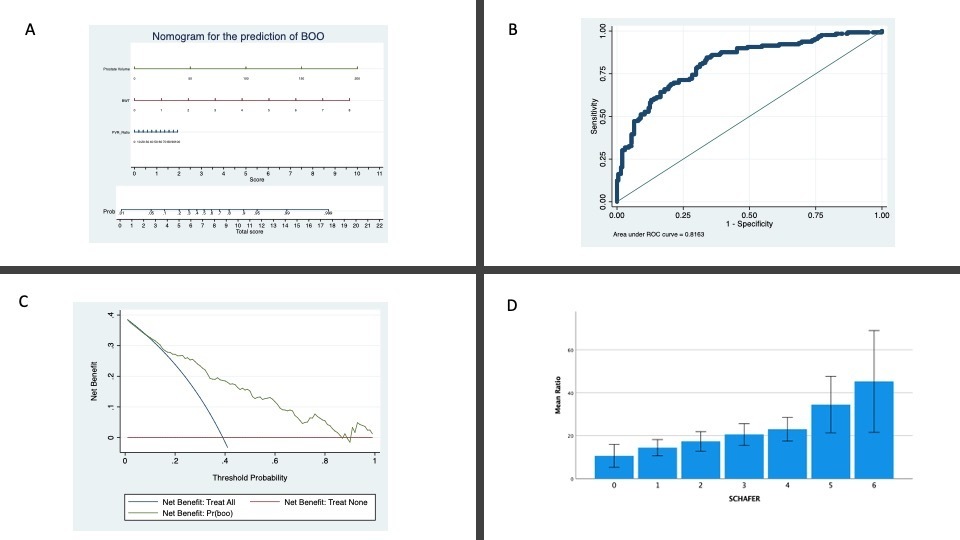
Introduction: Recently some authors have suggested a possible role of post-void residual ratio to predict bladder outlet obstruction (BOO). Aim of our study is to confirm the correlation between post-void residual urine ratio (PVR-R) and BOO diagnosed by pressure-flow studies (PFS) in males with lower urinary tract symptoms (LUTS) and to develop a clinical nomogram.
Methods: A consecutive series of patients aged 45 years or older with non-neurogenic LUTS were prospectively enrolled. Patients underwent standard diagnostic assessment for BOO including International Prostatic Symptoms Score, uroflowmetry, urodynamic studies (cystometry and pressure-flow studies), suprapubic ultrasound of the prostate and ultrasound measurements of the bladder wall thickness (BTW). PVR urine and the percentage of PVR to bladder volume (voided volume+PVR) (PVR-R) were evaluated. Logistic regression analysis was used to investigate predictors of pathological bladder emptying (BOO) defined as Schafer >II. Correlations were evaluated with Pearson test. A nomogram to predict BOO based on the multivariable logistic regression model was then developed. Discrimination and net benefit of the model was evaluated.
Results: Overall 335 patients with a mean age of 66 ± 11 years were enrolled. Overall, 131/335 (40%) presented BOO on PFS. Shaefer class was correlated with PVR-ratio with a Pearson coefficient of 0,297 (Figure). In a multivariable logistic age-adjusted regression model BWT (odds ratio [OR]: 2,21 per mm; 95% confidence interval [CI], 1,57-3,11; p = .001), PVR-R (OR: 1,01 per mL/s; 95% CI, 1,00-1,03; p = .046) and prostate volume (OR: 1,03 per mL/s; 95% CI, 1,03-1,06; p = .001) were significant predictors for BOO. The model presented an accuracy of 0,82 and a clinical net benefit in the range of 10-90%.
Figure: A Nomogram, B: ROC curve, C: Decision Curve Analysis, D: Median PVR_ratios in different Shaffer classes.
Conclusions: The present study confirms the important role of PVR-ratio in the prediction of BOO. For the first time we present a clinical nomogram including PVR-ratio for the prediction of BOO. Eternal validation is needed before clinical implementation.
Source of Funding: None.
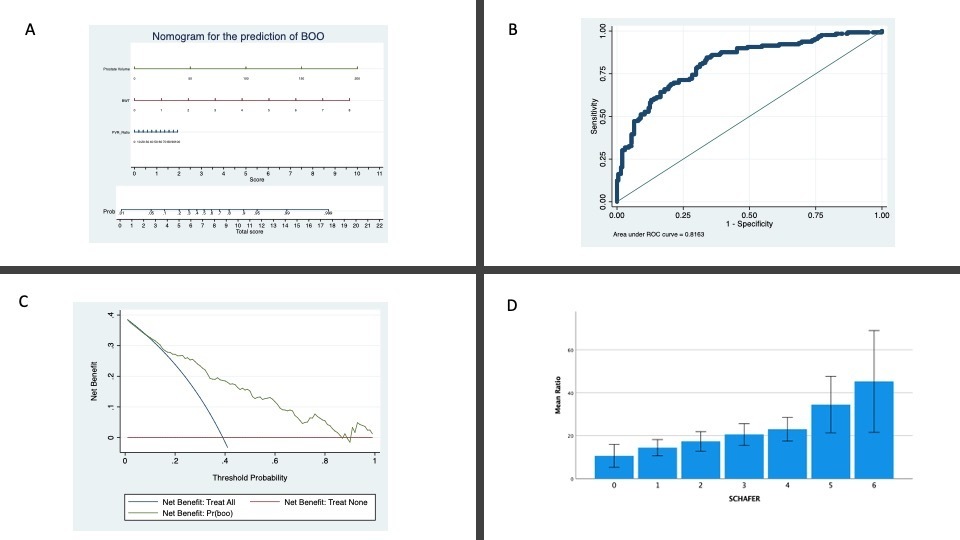
Methods: A consecutive series of patients aged 45 years or older with non-neurogenic LUTS were prospectively enrolled. Patients underwent standard diagnostic assessment for BOO including International Prostatic Symptoms Score, uroflowmetry, urodynamic studies (cystometry and pressure-flow studies), suprapubic ultrasound of the prostate and ultrasound measurements of the bladder wall thickness (BTW). PVR urine and the percentage of PVR to bladder volume (voided volume+PVR) (PVR-R) were evaluated. Logistic regression analysis was used to investigate predictors of pathological bladder emptying (BOO) defined as Schafer >II. Correlations were evaluated with Pearson test. A nomogram to predict BOO based on the multivariable logistic regression model was then developed. Discrimination and net benefit of the model was evaluated.
Results: Overall 335 patients with a mean age of 66 ± 11 years were enrolled. Overall, 131/335 (40%) presented BOO on PFS. Shaefer class was correlated with PVR-ratio with a Pearson coefficient of 0,297 (Figure). In a multivariable logistic age-adjusted regression model BWT (odds ratio [OR]: 2,21 per mm; 95% confidence interval [CI], 1,57-3,11; p = .001), PVR-R (OR: 1,01 per mL/s; 95% CI, 1,00-1,03; p = .046) and prostate volume (OR: 1,03 per mL/s; 95% CI, 1,03-1,06; p = .001) were significant predictors for BOO. The model presented an accuracy of 0,82 and a clinical net benefit in the range of 10-90%.
Figure: A Nomogram, B: ROC curve, C: Decision Curve Analysis, D: Median PVR_ratios in different Shaffer classes.
Conclusions: The present study confirms the important role of PVR-ratio in the prediction of BOO. For the first time we present a clinical nomogram including PVR-ratio for the prediction of BOO. Eternal validation is needed before clinical implementation.
Source of Funding: None.

.jpg)
.jpg)