Back
Poster, Podium & Video Sessions
Podium
PD40: Uroradiology II
PD40-05: Deep Learning Based Assessment of Prostate Lesion Dynamics on Multiparametric MRI During Active Surveillance
Sunday, May 15, 2022
10:10 AM – 10:20 AM
Location: Room 252
Michael Daneshvar*, Stephanie Harmon, Tim Phelps, Michael Rothberg, Jacob Enders, Nitin Yerram, Luke O'Connor, Alex Wang, Sherif Mehralivand, Samira Masoudi, Bethesda, MD, Dong Yang, Ziyue Xu, Daguang Xu, Santa Clara, CA, Maria Merino, Bradford Wood, Peter Choyke, Peter Pinto, Baris Turkbey, Bethesda, MD
- MD
Podium Presenter(s)
Introduction: For patients undergoing Active Surveillance (AS) for prostate cancer, the utility of longitudinal multiparametric MRI (mpMRI) is not well characterized. Given known inter-/intra-reader variability, a reproducible methodology for tracking intra-prostatic disease during AS is desired. We sought to utilize a deep learning (DL) detection and grading system to automatically assess lesion dynamics on mpMRI of AS patients and correlate findings with progression.
Methods: 49 patients undergoing mpMRI during AS were selected based on the following inclusion criteria: at least 3 consecutive scans (>6 months apart) with confirmatory biopsy. Progression was based on pathologic upgrading (n=24 patients). From each mpMRI acquisition, data from T2-weighted series and diffusion-weighted series were fed into a previously developed DL system which automatically segments intra-prostatic lesions and assigns imaging-based risk (high risk vs low risk trained from PI-RADS classifications). For each time point, the number of lesions, volume of lesions, and imaging-based risk category output. Total lesion volume growth/year was calculated. Cox proportional hazard regression analysis was used to assess correlation of DL-based output with disease progression.
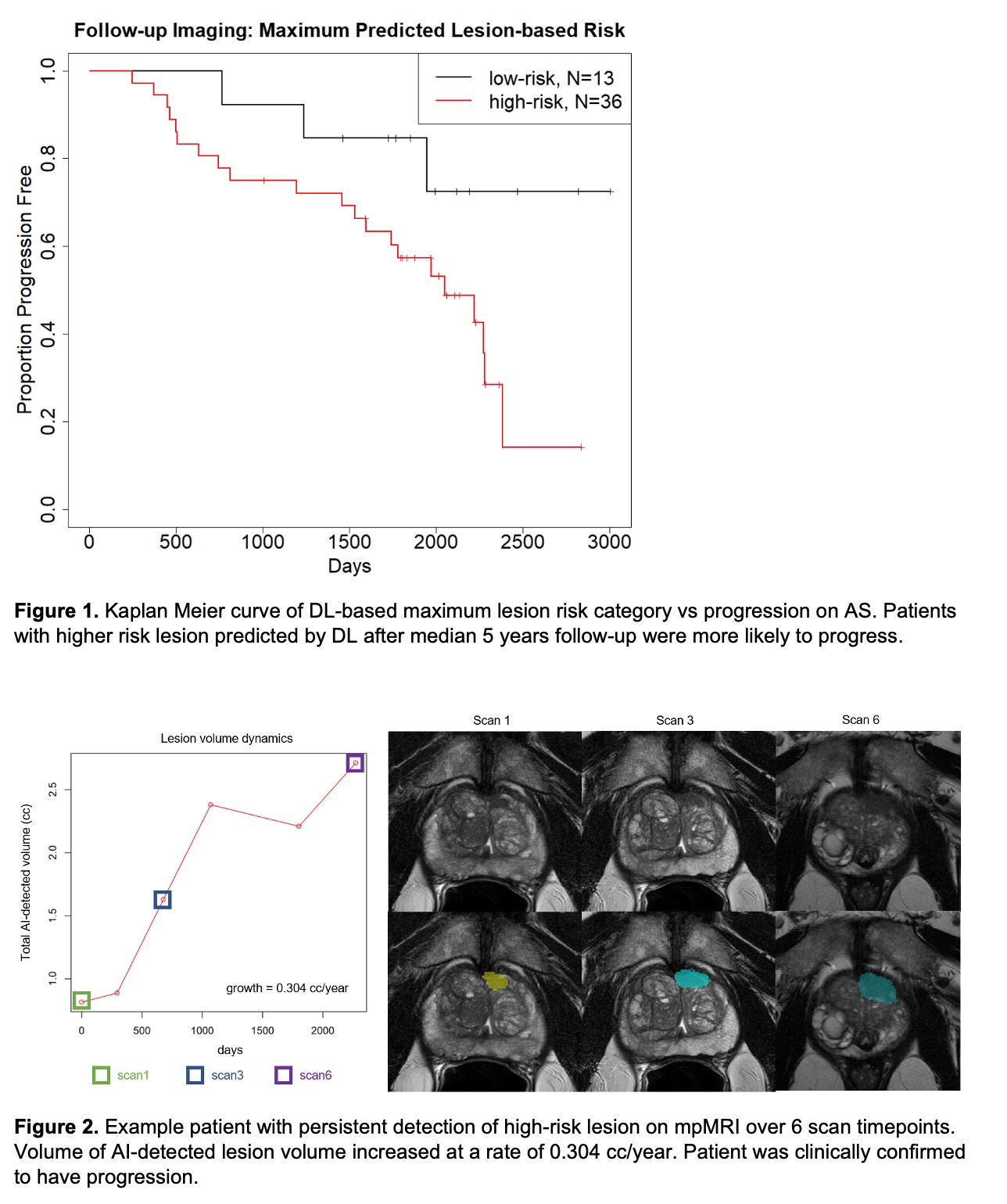
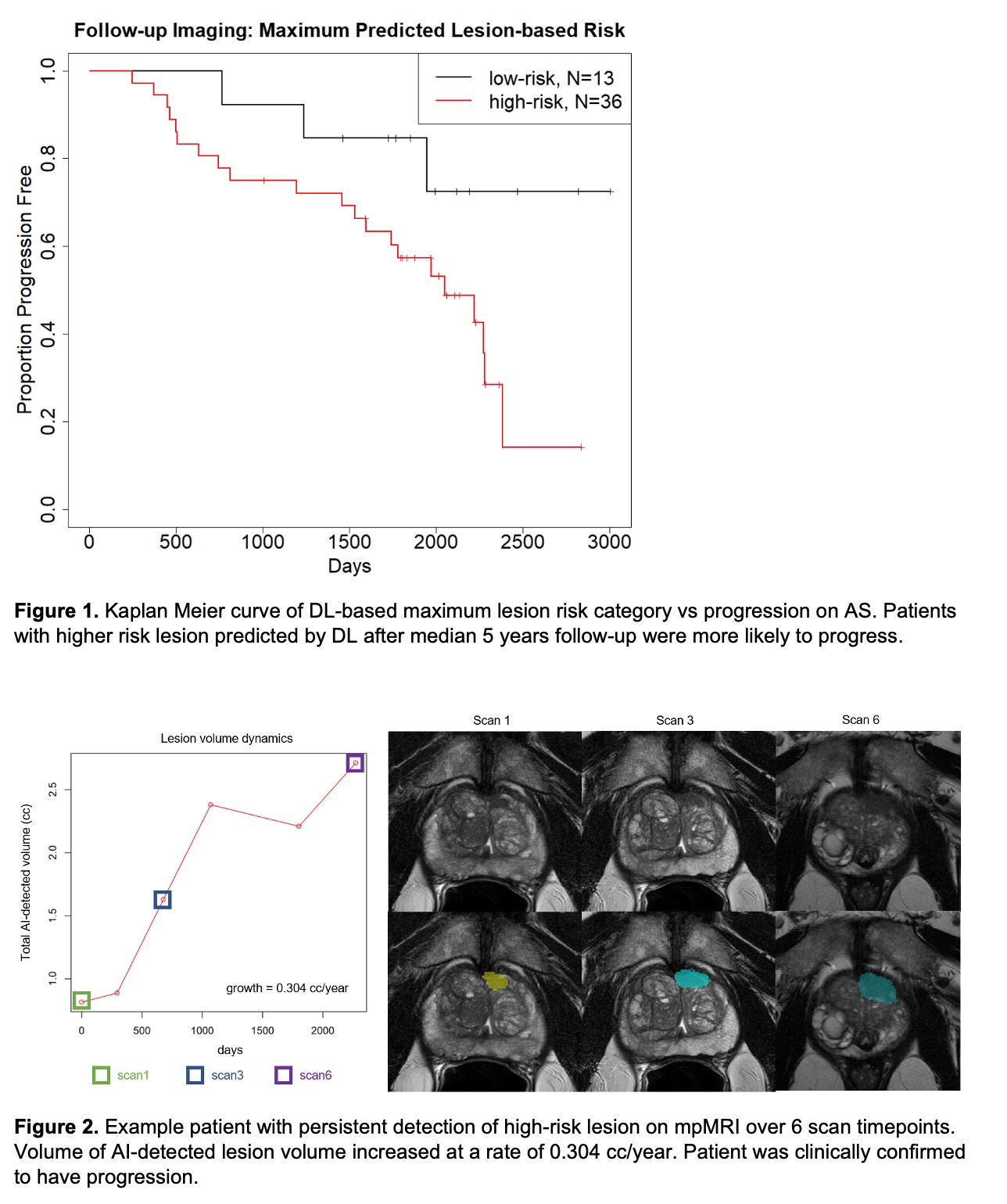
Results: Patients underwent a median of 4 scans (range 2-6) over a median period of 5 years (range 8.1 months to 8.2 years). There were no significant differences between progressors and non-progressors in DL-based lesion, lesion burden, or maximum risk scores at baseline. At final follow-up, progressors were characterized by increased number with high-risk lesions (21/24 vs 15/25, p=0.05) and burden of disease (0.022 [range 0,0.06] vs 0.007 [range 0,0.1], p=0.08) to non-progressors. Progressors experienced a median 0.17 cc/year tumor growth rate compared to 0.04 cc/year in non-progressors (p=0.35). Finally, patients harboring persistent high-risk lesions on follow-up imaging were at higher risk of progression (HR=3.3 [95%-CI:0.98-11], log-rank p=0.04).
Conclusions: DL-based tools for detection and grading of intraprostatic lesions on mpMRI can be used for fully automated characterization of disease dynamics during AS. Patients with aggressive features predicted by DL were more likely to progress off AS.
Source of Funding: The National Institute of Health (NIH) Medical Research Scholars Program, Foundation for the NIH, NIH Intramural Research Program
Methods: 49 patients undergoing mpMRI during AS were selected based on the following inclusion criteria: at least 3 consecutive scans (>6 months apart) with confirmatory biopsy. Progression was based on pathologic upgrading (n=24 patients). From each mpMRI acquisition, data from T2-weighted series and diffusion-weighted series were fed into a previously developed DL system which automatically segments intra-prostatic lesions and assigns imaging-based risk (high risk vs low risk trained from PI-RADS classifications). For each time point, the number of lesions, volume of lesions, and imaging-based risk category output. Total lesion volume growth/year was calculated. Cox proportional hazard regression analysis was used to assess correlation of DL-based output with disease progression.
Results: Patients underwent a median of 4 scans (range 2-6) over a median period of 5 years (range 8.1 months to 8.2 years). There were no significant differences between progressors and non-progressors in DL-based lesion, lesion burden, or maximum risk scores at baseline. At final follow-up, progressors were characterized by increased number with high-risk lesions (21/24 vs 15/25, p=0.05) and burden of disease (0.022 [range 0,0.06] vs 0.007 [range 0,0.1], p=0.08) to non-progressors. Progressors experienced a median 0.17 cc/year tumor growth rate compared to 0.04 cc/year in non-progressors (p=0.35). Finally, patients harboring persistent high-risk lesions on follow-up imaging were at higher risk of progression (HR=3.3 [95%-CI:0.98-11], log-rank p=0.04).
Conclusions: DL-based tools for detection and grading of intraprostatic lesions on mpMRI can be used for fully automated characterization of disease dynamics during AS. Patients with aggressive features predicted by DL were more likely to progress off AS.
Source of Funding: The National Institute of Health (NIH) Medical Research Scholars Program, Foundation for the NIH, NIH Intramural Research Program

.jpg)
.jpg)