Back
Poster, Podium & Video Sessions
Podium
PD40: Uroradiology II
PD40-07: Clinical Decision Algorithm using Restriction Spectrum Imaging and Biomarkers to Predict Upgrading in Active Surveillance
Sunday, May 15, 2022
10:30 AM – 10:40 AM
Location: Room 252
Stefan Eng, Los Angeles, CA, Benjamin Basasie, San Antonio, TX, Alfonso Lam, Los Angeles, CA, John Semmes, Dean Troyer, Norfolk, VA, Geoffrey Clarke, Abhijit Sunnapwar, Robin Leach, Teresa Johnson-Pais, San Antonio, TX, Lori Sokoll, Daniel Chan, Baltimore, MD, Jeffrey Tosoian, Javed Siddiqui, Arul Chinnaiyan, Ann Arbor, MI, Paul Boutros, Los Angeles, CA, Michael Liss*, San Antonio, TX

Michael A. Liss, MD,PhD,FACS,MS
University Of Texas Health San Antonio
Podium Presenter(s)
Introduction: To determine the relative value and optimal combination of radiologic and molecular biomarkers to predict prostate cancer progression in men on active surveillance.
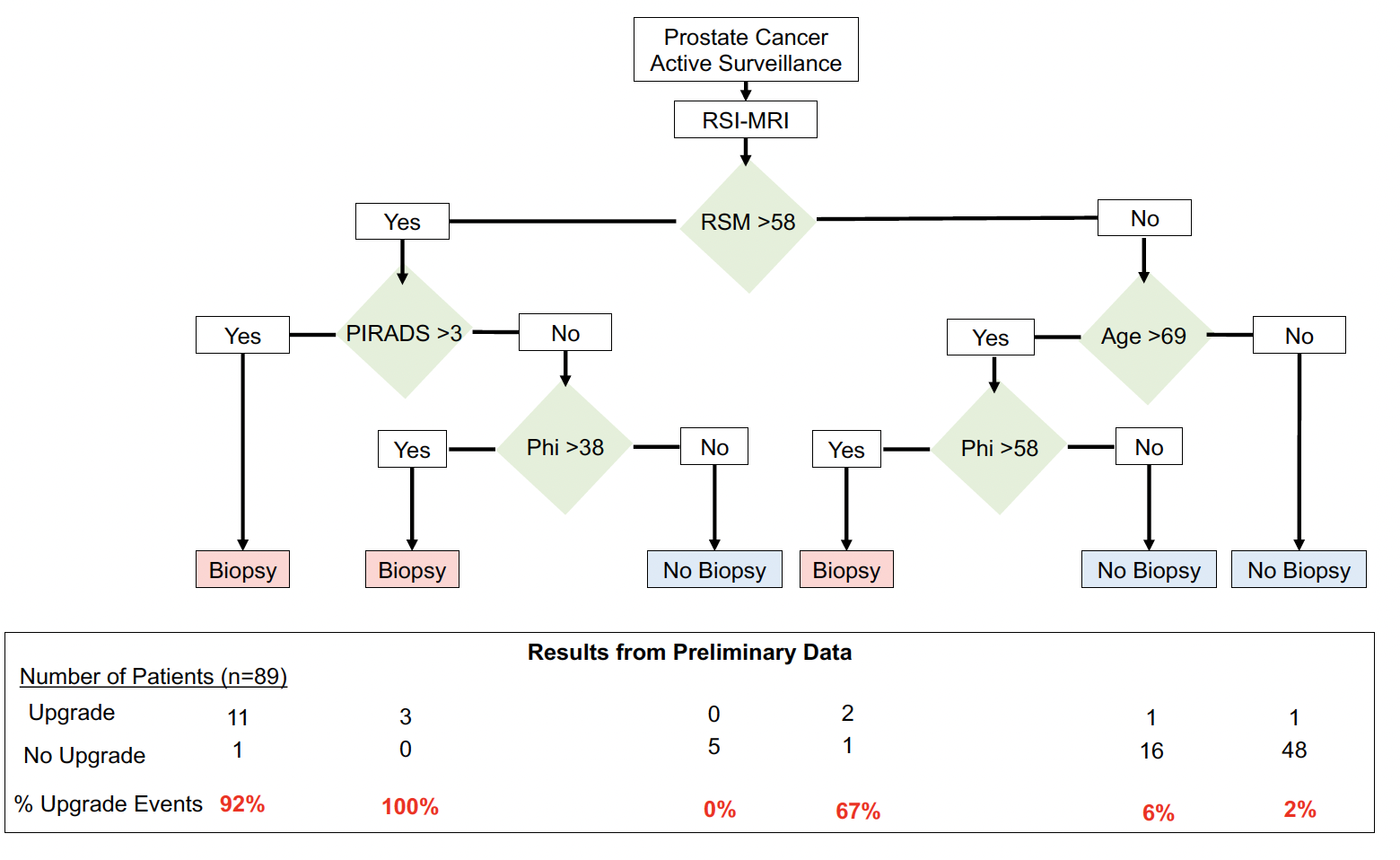
Methods: We prospectively enrolled 123 men with prostate cancer on active surveillance who were undergoing repeat biopsy to obtain an MRI and non-invasive biomarkers that predict the risk of upgrading. Subjects underwent a prostate multiparametric MRI and a short duration, diffusion-weighted enhanced MRI called restriction spectrum imaging (RSI) to generate a restricted signal map (RSM) along with evaluation of 30 features (14 clinico-epidemiologic features, 9 molecular biomarkers and 7 radiologic-associated features). Our primary outcome was upgrading to higher grade disease on subsequent active surveillance prostate biopsy. Statistical analysis evaluated AUROC and AUPRC, and improvements in these. Using the data, we then devised a clinical decision algorithm to best predict upgrading using the tested biomarkers.
Results: RSM (RSI-MRI biomarker) was the most accurate single biomarker in predicting upgrading at the subsequent active surveillance biopsy (AUROC = 0.84; 95%CI: 0.71-0.96). RSI improved a baseline clinical model that included MRI PIRADSv2 scores from an AUROC of 0.74 (95%CI 0.69-0.80) to 0.84 (95% CI 0.79 – 0.89). The best non-imaging biomarker was the prostate volume corrected Prostate Health Index (PHI) density (AUROC = 0.68; 95%CI: 0.53-0.82). Combining these with age as a clinical decision tree to perform or not perform a biopsy using cross validated statistics we reach an AUC of the model at 0.8 (SD 0.18)
Conclusions: Enhancement of diffusion-weighted imaging using RSI in addition to standard PIRADSv2 scoring, PHI, and age provides improvement to the predictive ability of MRI to detect upgrading in active surveillance. A combination of multiple biomarkers in a clinical decision tree improves prediction of groups at high risk for future upgrading.
Source of Funding: Department of Defense
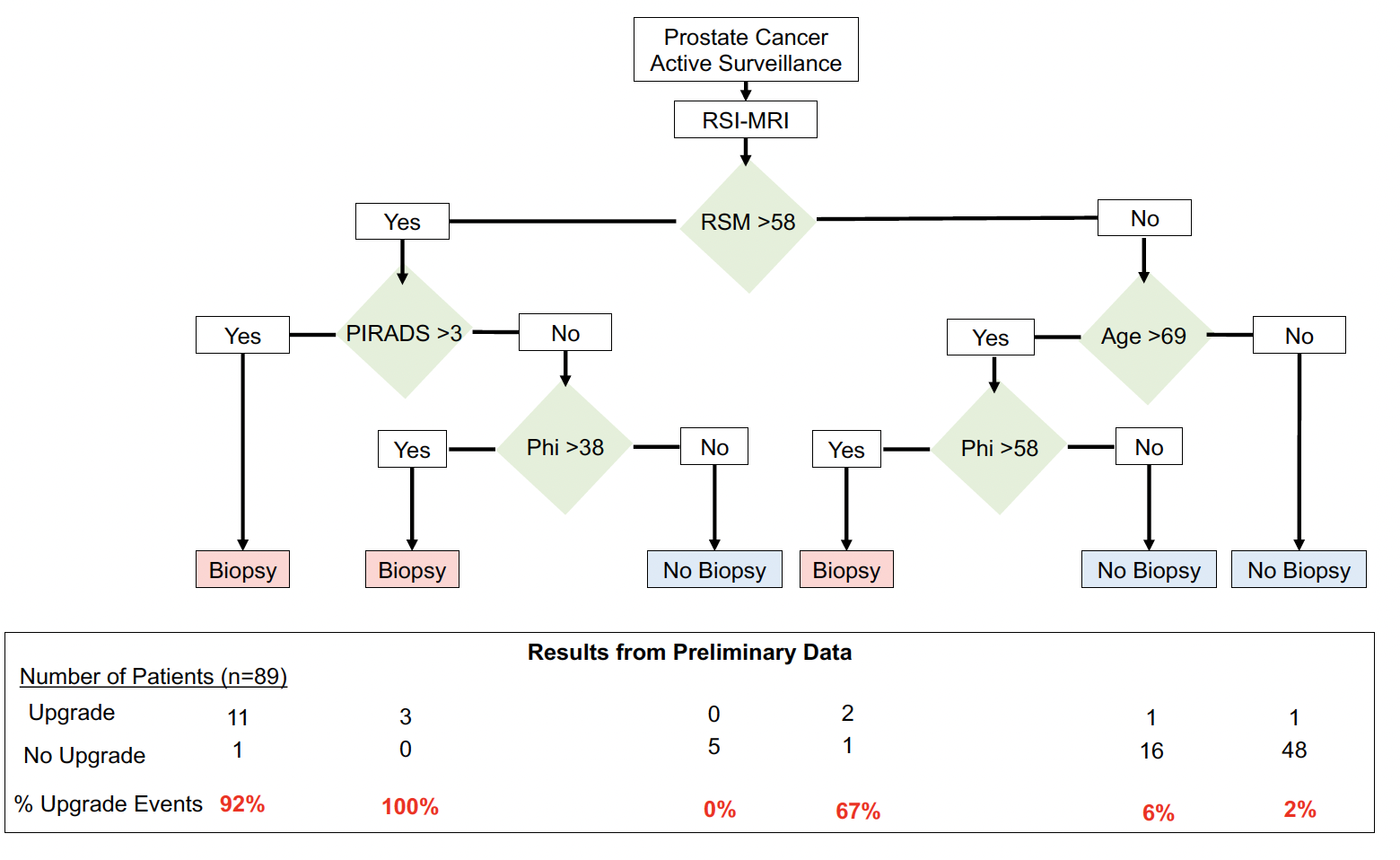
Methods: We prospectively enrolled 123 men with prostate cancer on active surveillance who were undergoing repeat biopsy to obtain an MRI and non-invasive biomarkers that predict the risk of upgrading. Subjects underwent a prostate multiparametric MRI and a short duration, diffusion-weighted enhanced MRI called restriction spectrum imaging (RSI) to generate a restricted signal map (RSM) along with evaluation of 30 features (14 clinico-epidemiologic features, 9 molecular biomarkers and 7 radiologic-associated features). Our primary outcome was upgrading to higher grade disease on subsequent active surveillance prostate biopsy. Statistical analysis evaluated AUROC and AUPRC, and improvements in these. Using the data, we then devised a clinical decision algorithm to best predict upgrading using the tested biomarkers.
Results: RSM (RSI-MRI biomarker) was the most accurate single biomarker in predicting upgrading at the subsequent active surveillance biopsy (AUROC = 0.84; 95%CI: 0.71-0.96). RSI improved a baseline clinical model that included MRI PIRADSv2 scores from an AUROC of 0.74 (95%CI 0.69-0.80) to 0.84 (95% CI 0.79 – 0.89). The best non-imaging biomarker was the prostate volume corrected Prostate Health Index (PHI) density (AUROC = 0.68; 95%CI: 0.53-0.82). Combining these with age as a clinical decision tree to perform or not perform a biopsy using cross validated statistics we reach an AUC of the model at 0.8 (SD 0.18)
Conclusions: Enhancement of diffusion-weighted imaging using RSI in addition to standard PIRADSv2 scoring, PHI, and age provides improvement to the predictive ability of MRI to detect upgrading in active surveillance. A combination of multiple biomarkers in a clinical decision tree improves prediction of groups at high risk for future upgrading.
Source of Funding: Department of Defense

.jpg)
.jpg)