Back
Poster, Podium & Video Sessions
Podium
PD41: Prostate Cancer: Detection & Screening IV
PD41-04: Distribution of National Comprehensive Cancer Network Risk Classifications Using Magnetic Resonance Imaging-Ultrasound Fusion versus Systemic 12 core Biopsies
Sunday, May 15, 2022
10:00 AM – 10:10 AM
Location: Room 255
Ghazal Khajir*, Benjamin Press, Preston Sprenkle, New Haven, CT, Samuel Washington, Matthew Cooperberg, San Francisco, CA, Michael Leapman, New Haven, CT
- GK
Ghazal Khajir, MD
Associate research scientist
Department of Urology, Yale school of medicine
Podium Presenter(s)
Introduction: The National Comprehensive Cancer Network (NCCN) risk criteria for prostate cancer are impactful when assessing suitability for active surveillance versus treatment for low-grade prostate cancer. However, in the contemporary era, few patients may meet stringent “very-low risk” criteria due in large part to improved sampling achieved through MRI-guided approaches, and may therefore drive over-treatment.
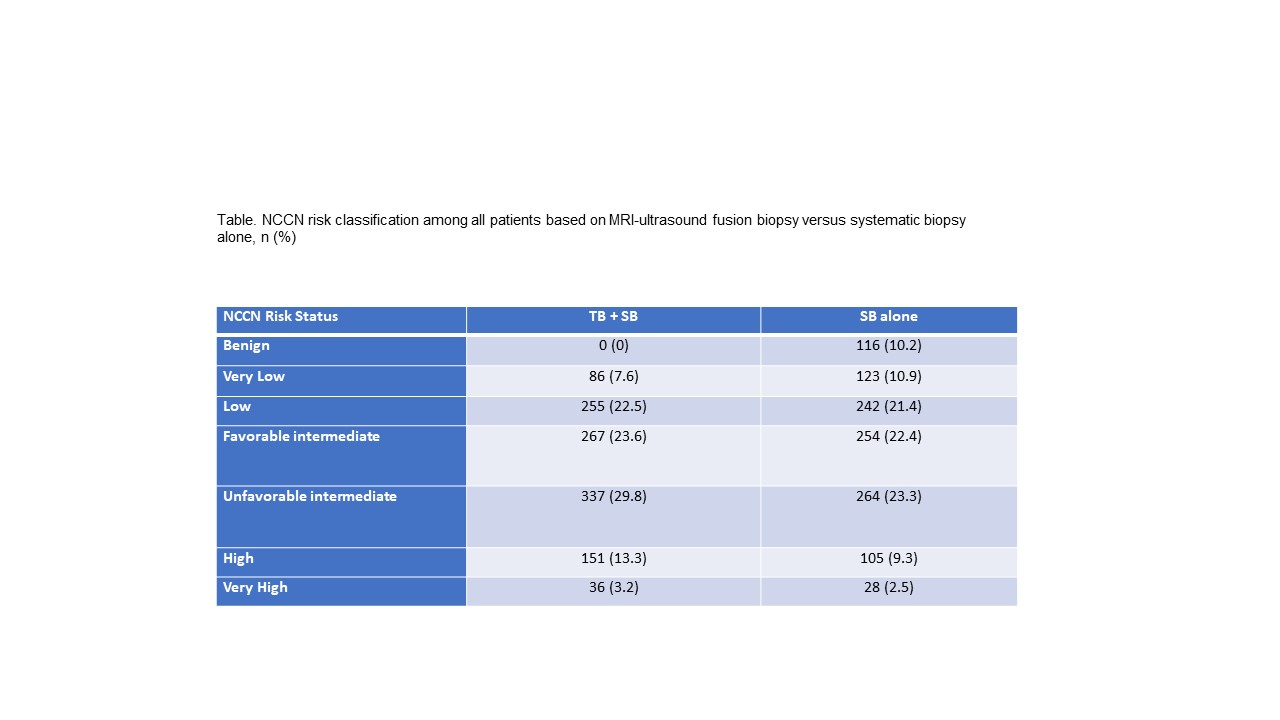
Methods: We performed a retrospective study of patients who underwent prostate MRI-ultrasound fusion biopsy at a single institution from January 2017 to July 2021. The primary study objective was to define the proportion of patients meeting NCCN “very-low risk” designation obtained using MRI-ultrasound fusion (systematic + targeted) versus systemic 12 core biopsy (SB). We calculated NCCN risk classifications (very low, low, favorable intermediate, unfavorable intermediate, high, and very high) based on constituent components (PSA, PSA density, number of biopsy cores positive, greatest extent of core positivity). We conducted comparisons within patients based on findings obtained through MRI-ultrasound fusion biopsy versus SB only.
Results: We identified 1,132 patients, including 1,014 (89.5%%) and 118 (10.5%) who underwent first-time biopsy and surveillance biopsies. The median PSA was 7.2 ng/mL (interquartile range: 5.3-10.8). Using data obtained through systematic biopsy alone, 123 (10.9%) and 242 (21.4%) were classified as very-low and low NCCN risk, respectively. Incorporating data from MRI-ultrasound fusion biopsy, 86 (7.6%) and 255 (22.5%) were classified as very-low and low NCCN risk, respectively. Among patients initially electing active surveillance as management, 7.4%, 60.2%, 26.9% met very-low, low, and favorable-intermediate risk criteria, respectively.
Conclusions: A very small proportion of patients undergoing MRI-ultrasound fusion biopsy will be classified as “very-low risk” by the NCCN definition, and the majority of patients managed appropriately with active surveillance do not meet these criteria. These findings imply a need to broaden support for active surveillance outside of “very-low risk” criteria to promote greater uptake.
Source of Funding: N/A
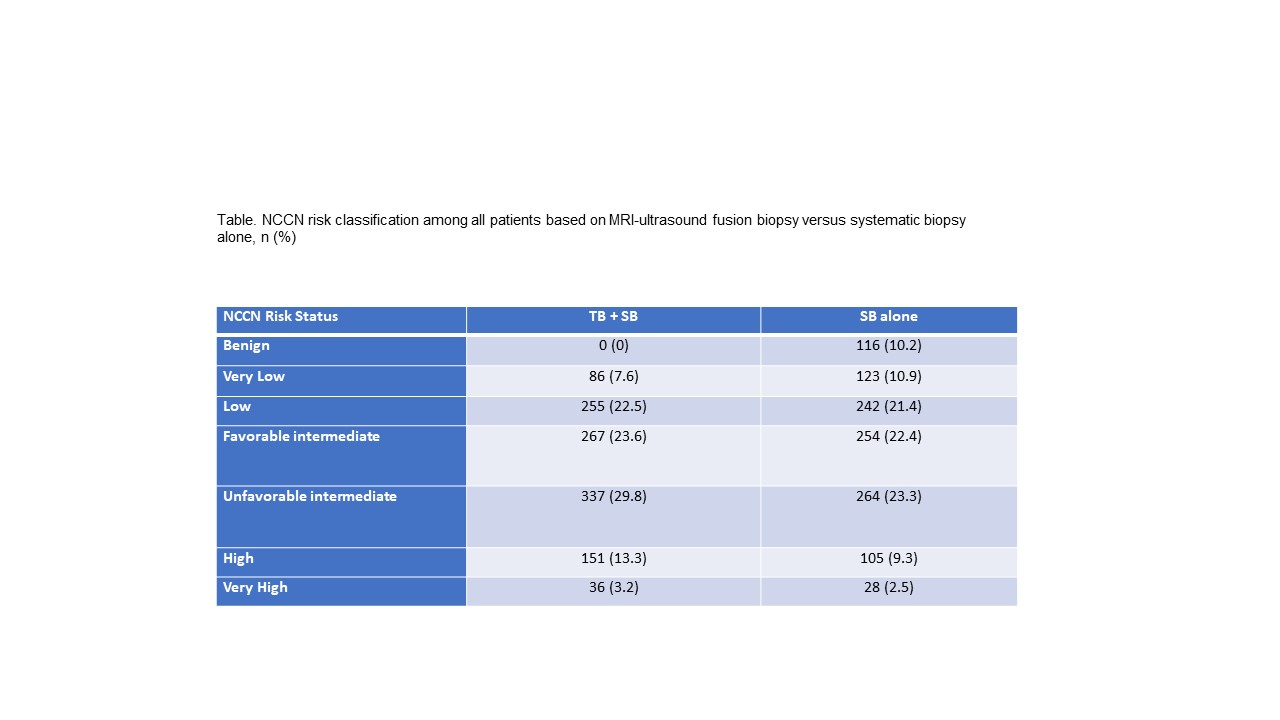
Methods: We performed a retrospective study of patients who underwent prostate MRI-ultrasound fusion biopsy at a single institution from January 2017 to July 2021. The primary study objective was to define the proportion of patients meeting NCCN “very-low risk” designation obtained using MRI-ultrasound fusion (systematic + targeted) versus systemic 12 core biopsy (SB). We calculated NCCN risk classifications (very low, low, favorable intermediate, unfavorable intermediate, high, and very high) based on constituent components (PSA, PSA density, number of biopsy cores positive, greatest extent of core positivity). We conducted comparisons within patients based on findings obtained through MRI-ultrasound fusion biopsy versus SB only.
Results: We identified 1,132 patients, including 1,014 (89.5%%) and 118 (10.5%) who underwent first-time biopsy and surveillance biopsies. The median PSA was 7.2 ng/mL (interquartile range: 5.3-10.8). Using data obtained through systematic biopsy alone, 123 (10.9%) and 242 (21.4%) were classified as very-low and low NCCN risk, respectively. Incorporating data from MRI-ultrasound fusion biopsy, 86 (7.6%) and 255 (22.5%) were classified as very-low and low NCCN risk, respectively. Among patients initially electing active surveillance as management, 7.4%, 60.2%, 26.9% met very-low, low, and favorable-intermediate risk criteria, respectively.
Conclusions: A very small proportion of patients undergoing MRI-ultrasound fusion biopsy will be classified as “very-low risk” by the NCCN definition, and the majority of patients managed appropriately with active surveillance do not meet these criteria. These findings imply a need to broaden support for active surveillance outside of “very-low risk” criteria to promote greater uptake.
Source of Funding: N/A

.jpg)
.jpg)