Back
Poster, Podium & Video Sessions
Podium
PD42: Bladder Cancer: Invasive IV
PD42-10: Independent Predictors and Patterns of Early and Late Recurrence after Radical Cystectomy for Bladder Cancer: a Multicenter Collaboration
Sunday, May 15, 2022
11:00 AM – 11:10 AM
Location: Room 245
Chiara Lonati*, Brescia, Italy, Roberto Carando, Lucerne, Switzerland, Alberto Martini, Milan, Italy, Claudio Simeone, Stefania Zamboni, Brescia, Italy, Giuseppe Simone, Rome, Italy, Luca Afferi, Christian D. Fankhauser, Agostino Mattei, Lucerne, Switzerland, Mario Álvarez-Maestro, Madrid, Spain, Alberto Briganti, Francesco Montorsi, Marco Moschini, Milan, Italy

Chiara Lonati, MD
Spedali Civili of Brescia
Podium Presenter(s)
Introduction: Sparce evidence exists regarding risk factors for tumor recurrence after radical cystectomy (RC) for bladder cancer (BCa). We aimed to assess independent predictors of early and late recurrence after RC and to analyze patterns of recurrence, in order to tailor a personalized follow-up protocol according to individual features
Methods: We retrospectively analyzed data of 1,894 patients treated with RC. Considering a 3-year threshold value for the definition of late recurrence, patients with follow-up shorter than 3-year were excluded. The final cohort included 863 patients treated with RC for BCa at 4 tertiary referral centers between 2013 and 2017. Recurrence was coded as early ( <3 years) and late (>3 years). Recurrence was coded as local (cystectomy bed or pelvic lymph node [LN] dissection template), urothelial (upper urinary tract and urethral carcinoma), and distant (including non-regional LNs) recurrence according to location. Multivariable Cox regression models were applied to predict risk of overall, early, and late recurrence; covariates consisted of clinical and pathological features
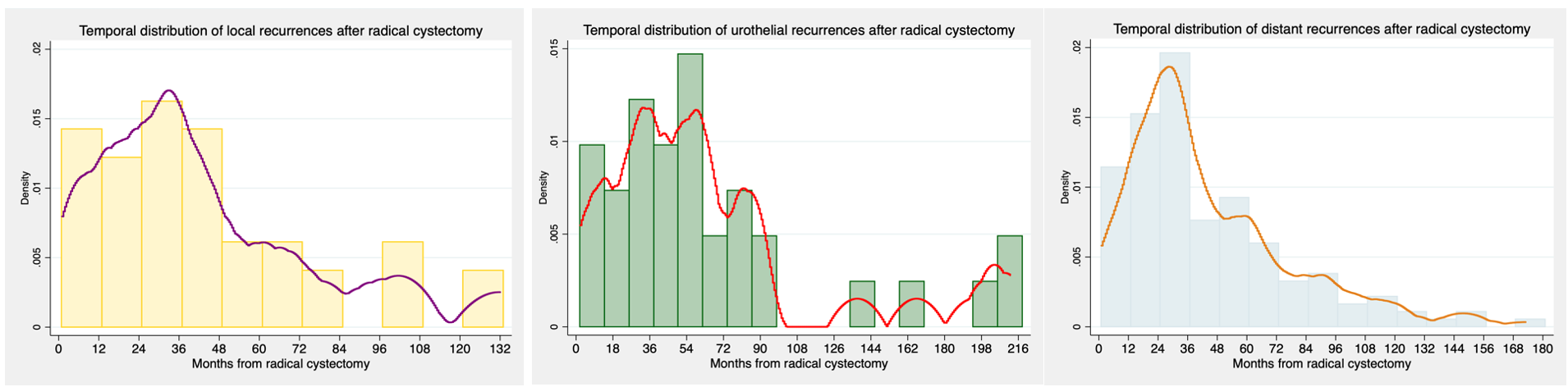
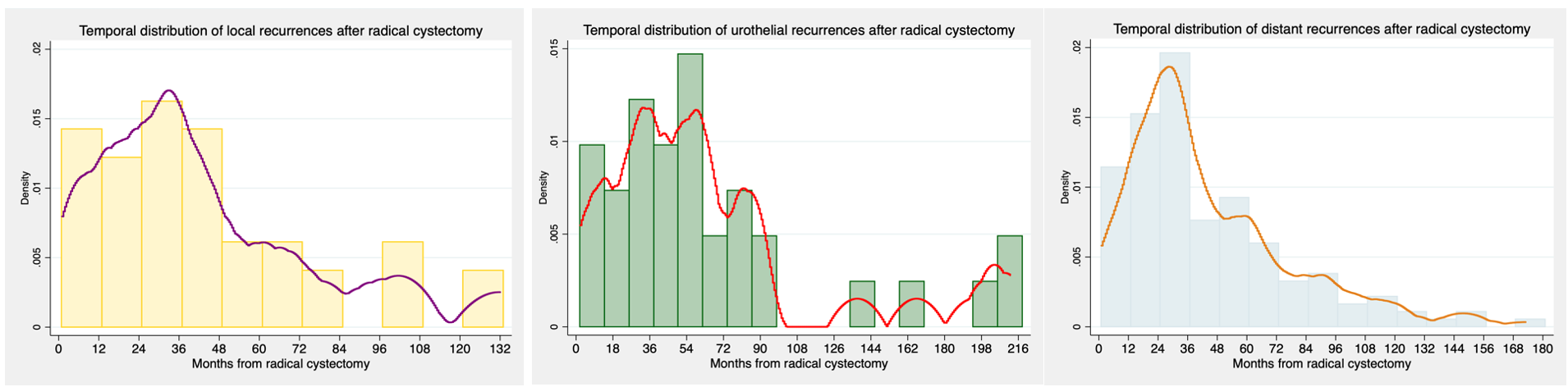
Results: Overall, 11.7% and 12.5% of patients experienced early (median time: 22 months) and late (median time: 60 months) recurrence, respectively. Fig.1 depicts temporal distribution of recurrence according to location, showing a high risk of local and distant recurrence until the second year and urothelial recurrence until the fifth year after RC. Early recurrence occurred in non-regional LNs in 45% of cases, followed by lung (41%), local (21%), and urothelial recurrence (11%), while distant recurrence involved non-regional LNs, lung, urothelial, and local recurrence in 34%, 33%, 21%, and 19% of cases, respectively. At multivariable Cox analyses, pT3/4 (hazard ratio [HR]: 1.58; p=0.03), pN+ (HR: 2.06; 0 <0.001), and positive surgical margins (HR: 2.03; p=0.04) were significantly associated with risk of overall recurrence, while pN+ and concomitant carcinoma in situ were independent predictors of early (HR: 3.00; p<0.001) and late (HR: 1.64; p=0.02) recurrence, respectively
Conclusions: Patients at increased risk for recurrence after RC should be referred to a stricter follow-up protocol, especially until the second year after RC and focused on distant recurrence
Source of Funding: None
Methods: We retrospectively analyzed data of 1,894 patients treated with RC. Considering a 3-year threshold value for the definition of late recurrence, patients with follow-up shorter than 3-year were excluded. The final cohort included 863 patients treated with RC for BCa at 4 tertiary referral centers between 2013 and 2017. Recurrence was coded as early ( <3 years) and late (>3 years). Recurrence was coded as local (cystectomy bed or pelvic lymph node [LN] dissection template), urothelial (upper urinary tract and urethral carcinoma), and distant (including non-regional LNs) recurrence according to location. Multivariable Cox regression models were applied to predict risk of overall, early, and late recurrence; covariates consisted of clinical and pathological features
Results: Overall, 11.7% and 12.5% of patients experienced early (median time: 22 months) and late (median time: 60 months) recurrence, respectively. Fig.1 depicts temporal distribution of recurrence according to location, showing a high risk of local and distant recurrence until the second year and urothelial recurrence until the fifth year after RC. Early recurrence occurred in non-regional LNs in 45% of cases, followed by lung (41%), local (21%), and urothelial recurrence (11%), while distant recurrence involved non-regional LNs, lung, urothelial, and local recurrence in 34%, 33%, 21%, and 19% of cases, respectively. At multivariable Cox analyses, pT3/4 (hazard ratio [HR]: 1.58; p=0.03), pN+ (HR: 2.06; 0 <0.001), and positive surgical margins (HR: 2.03; p=0.04) were significantly associated with risk of overall recurrence, while pN+ and concomitant carcinoma in situ were independent predictors of early (HR: 3.00; p<0.001) and late (HR: 1.64; p=0.02) recurrence, respectively
Conclusions: Patients at increased risk for recurrence after RC should be referred to a stricter follow-up protocol, especially until the second year after RC and focused on distant recurrence
Source of Funding: None

.jpg)
.jpg)