Back
Poster, Podium & Video Sessions
Podium
PD44: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Pelvic Prolapse
PD44-10: Urodynamic profile of voiding in pelvic organ prolapse patients after surgery: A systematic review with meta-analysis
Sunday, May 15, 2022
11:00 AM – 11:10 AM
Location: Room 243
Hugo Santos*, Danilo Lourenço, Alexandre Partezani, Saulo Teles, Lucas Takemura, Felipe Gushiken, Guilherme Andrade, Bianca Bianco, Luis Rios, Gustavo Lemos, Arie Carneiro, São Paulo, Brazil
- HO
Hugo Octaviano Santos, MD
Hospital Israelita Albert Einstein
Podium Presenter(s)
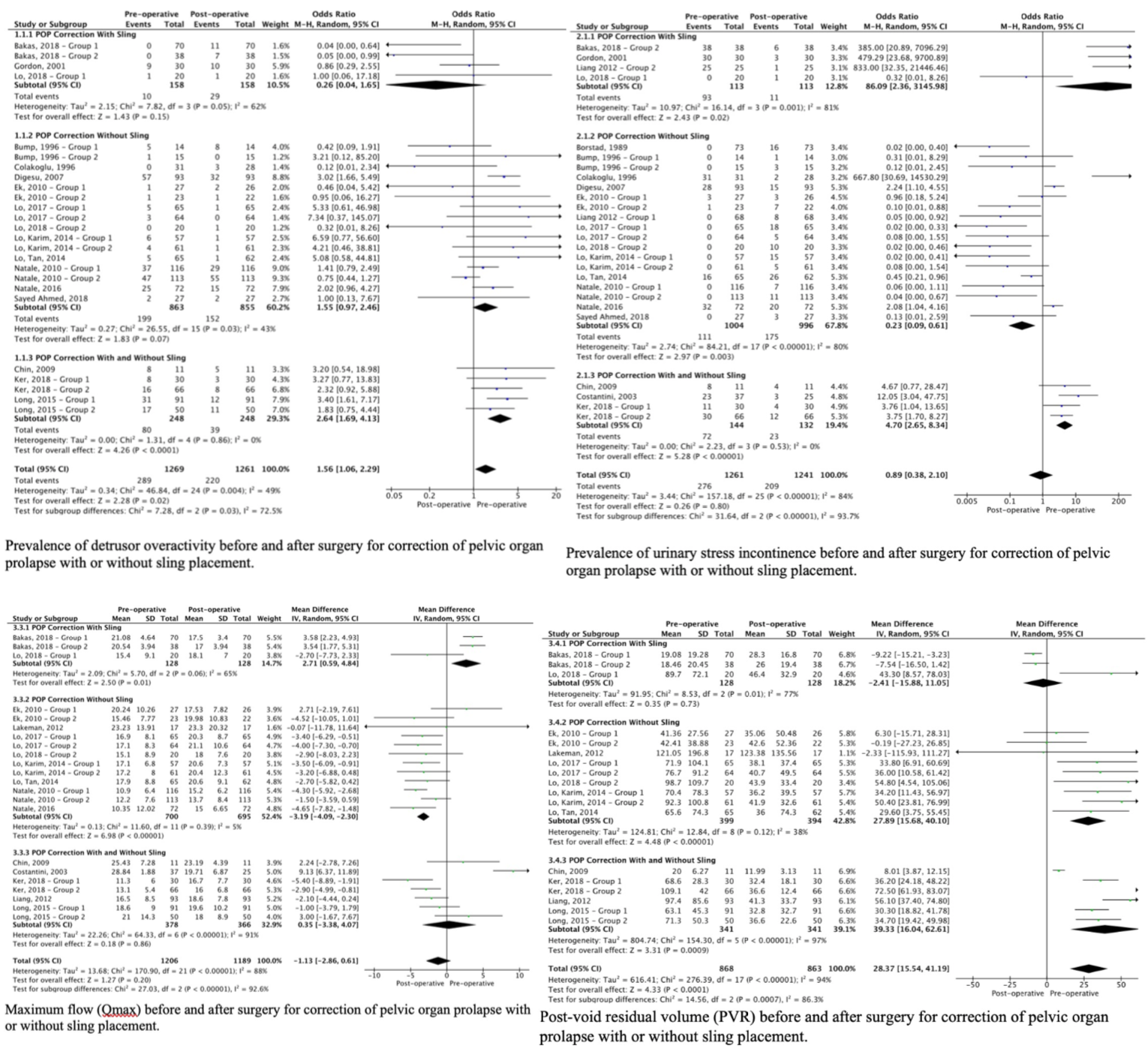
Introduction: Pelvic organ prolapse (POP) originates due to defects on the female pelvic floor and is a prevalent disorder in women. Stress urinary incontinence (SUI), urge urinary incontinence (UUI), and obstructive symptoms may concur in these patients. Surgical treatment of POP aims to restore the anatomy and function of the genitals; however, it may prompt urinary symptoms not presented previously. We aimed to perform a systematic review and meta-analysis of urodynamic changes in patients undergoing surgical correction for POP.
Methods: This study was conducted according to the PRISMA protocol. Studies in English, published from 1976 to July 2020 in Pubmed and Cochrane were included. Studies included contained data from urodynamic evaluation from before and after vaginal surgery for POP, with or without anti-incontinence procedures. The main urodynamic data collected were: (1) Free uroflowmetry: Qmax, voided volume, and PVR; (2) Cystometry: Bladder capacity, presence of DO, SUI or UUI and VLPP; (3) Pressure x flow study: PdetQmax, Qmax and PVR. Bias risk assessment was performed in all studies.
Results: 22 studies published between 1989 and 2018 were included, involving 1,549 women. MUS placement was assessed independently in 3 studies. Patients had a significantly higher prevalence of DO before surgery (OR 1.56, 95% CI 1.06-2.29; p=0.02), surgeries without sling placement demonstrated a tendency of ameliorating DO. Patients that did not receive sling were more incontinent after surgery, with a lower prevalence of SUI before surgery (OR 0.23, 95% CI 0.09-0.61; p=0.003). Bladder emptying parameters improved after surgery, with higher PdetQmax before surgery (IV 3.23, 95% CI 0.45-1.18; p=0.02). For patients that did not receive MUS, a lower Qmax (IV -3.19, 95% CI -4.09 - -2.30; p= <0.001) and a higher PVR (IV 27.89, 95% CI 15.68-40.1; p<0,001) was observed before surgery.
Conclusions: POP correction surgery yields better urodynamic emptying parameters, with a lower PdetQmax, higher Qmax and lower PVR. The procedure is associated with a reduction of detrusor overactivity. Sling placement enhances obstructive parameters. Patients significantly improve their symptoms with POP correction surgery.
Source of Funding: Not applicable
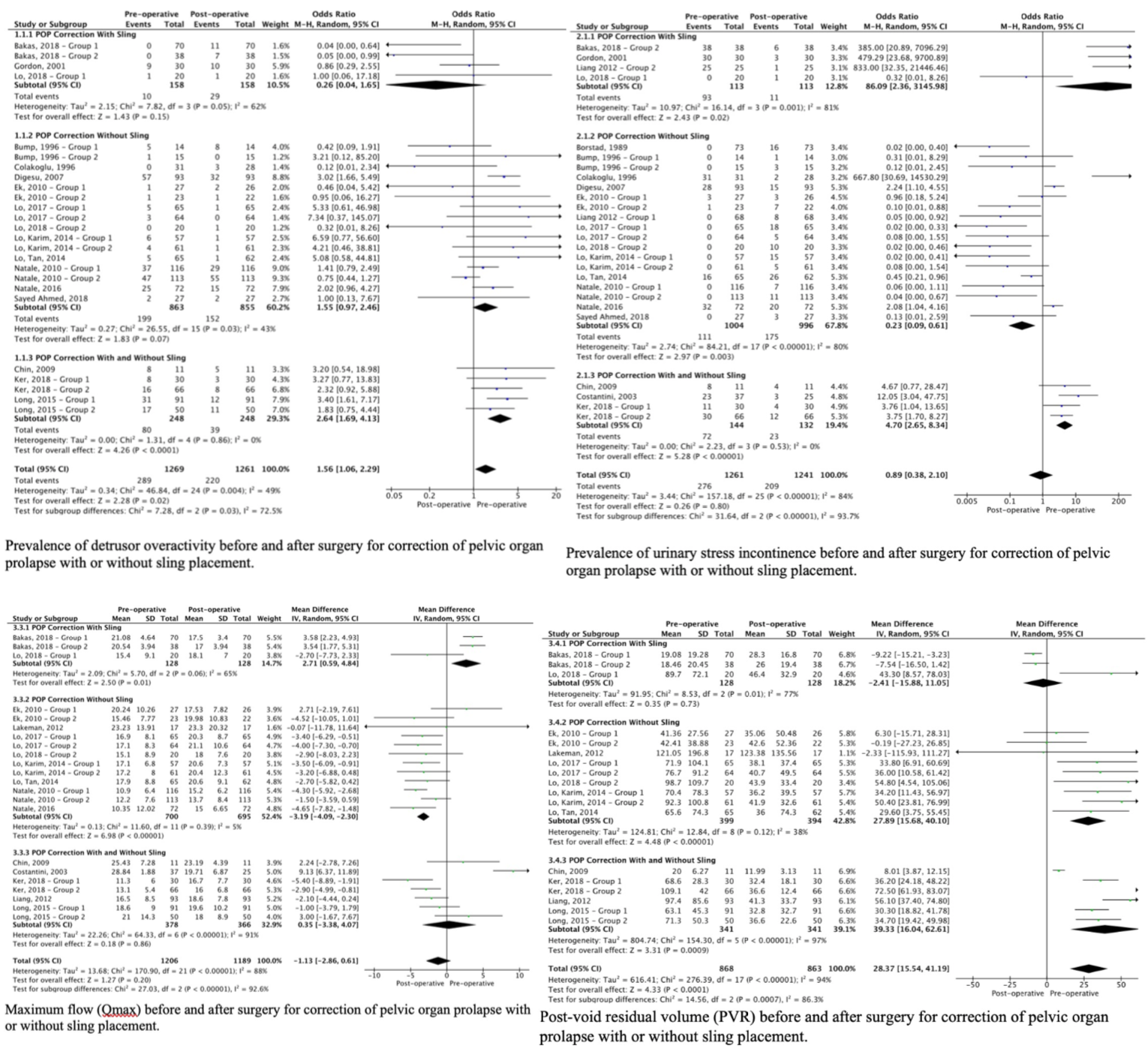
Methods: This study was conducted according to the PRISMA protocol. Studies in English, published from 1976 to July 2020 in Pubmed and Cochrane were included. Studies included contained data from urodynamic evaluation from before and after vaginal surgery for POP, with or without anti-incontinence procedures. The main urodynamic data collected were: (1) Free uroflowmetry: Qmax, voided volume, and PVR; (2) Cystometry: Bladder capacity, presence of DO, SUI or UUI and VLPP; (3) Pressure x flow study: PdetQmax, Qmax and PVR. Bias risk assessment was performed in all studies.
Results: 22 studies published between 1989 and 2018 were included, involving 1,549 women. MUS placement was assessed independently in 3 studies. Patients had a significantly higher prevalence of DO before surgery (OR 1.56, 95% CI 1.06-2.29; p=0.02), surgeries without sling placement demonstrated a tendency of ameliorating DO. Patients that did not receive sling were more incontinent after surgery, with a lower prevalence of SUI before surgery (OR 0.23, 95% CI 0.09-0.61; p=0.003). Bladder emptying parameters improved after surgery, with higher PdetQmax before surgery (IV 3.23, 95% CI 0.45-1.18; p=0.02). For patients that did not receive MUS, a lower Qmax (IV -3.19, 95% CI -4.09 - -2.30; p= <0.001) and a higher PVR (IV 27.89, 95% CI 15.68-40.1; p<0,001) was observed before surgery.
Conclusions: POP correction surgery yields better urodynamic emptying parameters, with a lower PdetQmax, higher Qmax and lower PVR. The procedure is associated with a reduction of detrusor overactivity. Sling placement enhances obstructive parameters. Patients significantly improve their symptoms with POP correction surgery.
Source of Funding: Not applicable

.jpg)
.jpg)