Back
Poster, Podium & Video Sessions
Podium
PD45: Benign Prostatic Hyperplasia: Surgical Therapy & New Technology IV
PD45-02: UroLift versus Rezum for Benign Prostatic Hyperplasia: a Real-World Single-Institution Analysis
Sunday, May 15, 2022
1:10 PM – 1:20 PM
Location: Room 252
Chih Peng Chin*, Evan Garden, Krishna Ravivarapu, Devki Shukla, Olamide Omidele, Micah Levy, Joseph Sewell Araya, New York, NY, Alexander Small, Bronx, NY, Steven Kaplan, Robert Valenzuela, Avinash Reddy, Susan Marshall, Jay Motola, Craig Nobert, Mantu Gupta, Michael Palese, New York, NY
- CC
Podium Presenter(s)
Introduction: UroLift and Rezum are newer minimally invasive BPH treatment options that have grown in popularity. Research directly comparing the two is limited. We report the largest cohort to date comparing real world clinical outcomes following UroLift and Rezum.
Methods: Patients at an academic institution between 1/2017 and 1/2021 were screened, and those with preoperative prostate volume >30cc and =80cc were included. Patients with follow-up <30 days were excluded. Outcomes included changes in AUA symptom score (AUA-SS), Qmax, post void residual (PVR), surgical retreatment rate, changes in BPH medications use, postoperative complications, ER visits, and readmissions within 90 days.
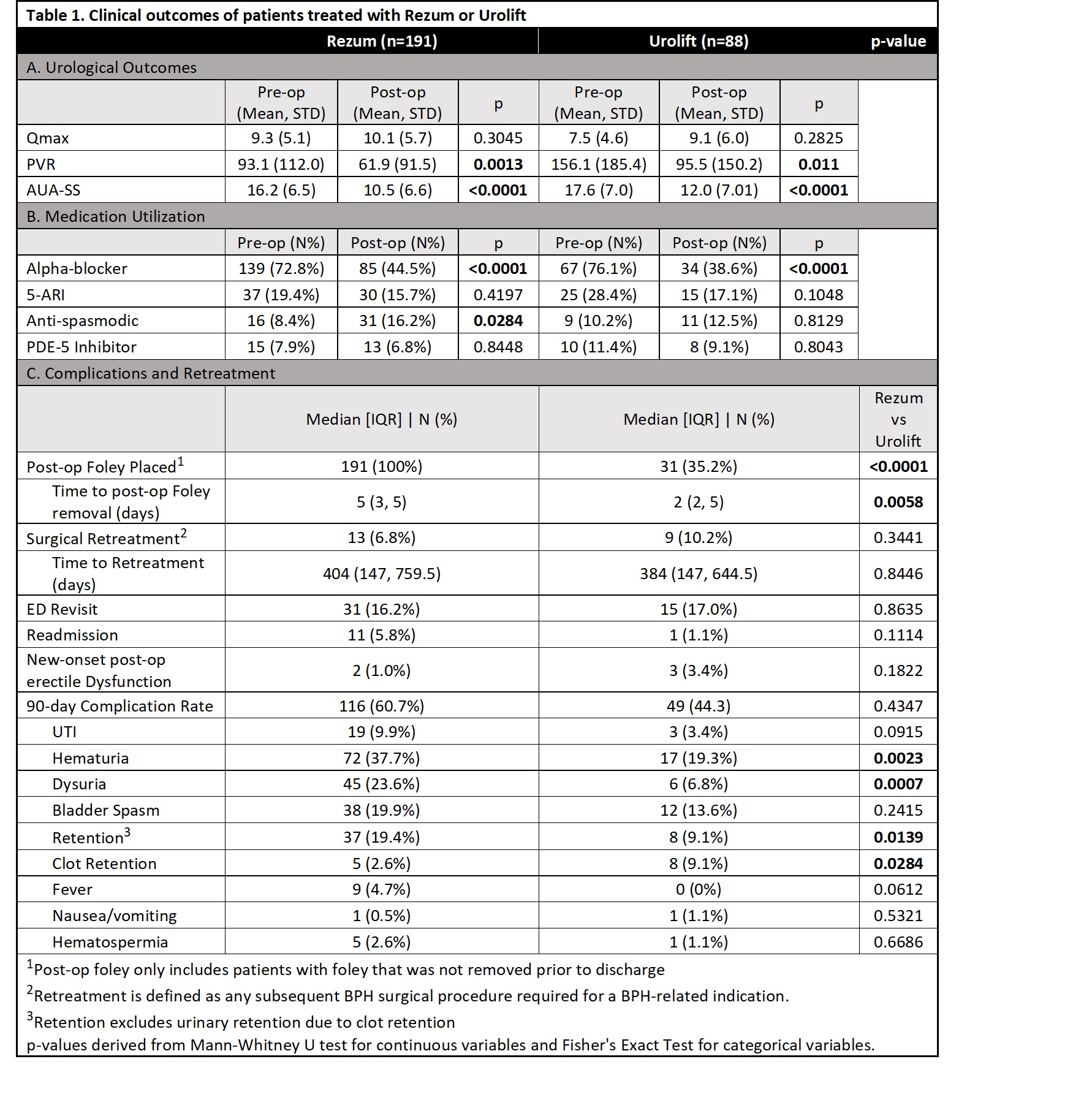
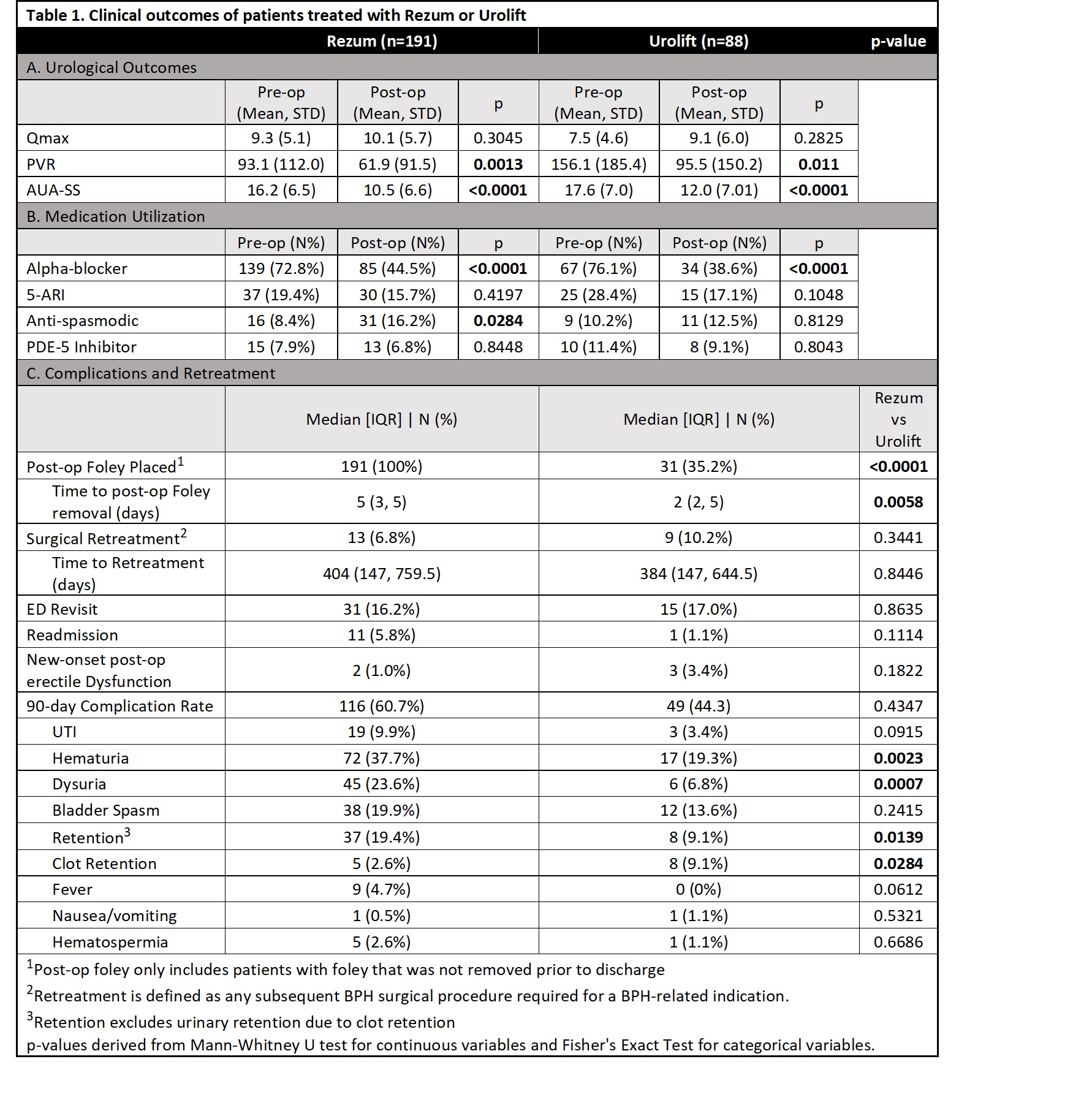
Results: We identified 375 Rezum and 151 UroLift patients of which 191 Rezum (51%) and 88 UroLift (58%) patients met inclusion criteria. Median follow-up for Rezum and UroLift patients was 173 and 307 days, respectively. Compared to Rezum patients, UroLift patients were older (Rezum 67 ± 8 vs UroLift 69 ± 9 years, p=0.014) and had smaller prostates (Rezum 50.7 ± 13.5 vs UroLift 44.9 ± 12.4 cc, p<0.001). Preoperatively, UroLift patients had higher PVR (Rezum 93 ± 112 vs Urolift 156 ± 185 mL, p=0.028) and lower Qmax (Rezum 9.3 ± 5.1 vs UroLift 7.5 ± 4.6 mL/sec, p=0.004). After treatment, both Rezum and UroLift patients had significant, similar improvements in AUA-SS (Rezum -4.0 ± 6.8 vs. UroLift -5.2 ± 8.0 points, p=0.349) and PVR (Rezum -26.5 ± 91.8 vs UroLift -59.3 ± 150.3 mL, p=0.349). There was no significant improvement in Qmax (Table 1a). Both groups had decreased alpha-blocker use after treatment (Rezum 72.8% to 44.5%, UroLift 76.1% to 38.6%, both p<0.001) (Table 1b). In the postoperative 90-day period, Rezum patients experienced more hematuria, dysuria and retention, whereas UroLift patients more frequently had clot retention (Table 1c). There were no differences in 90-day ER visits, 90-day readmissions, or surgical retreatment rates (all p>0.05).
Conclusions: For patients with BPH, UroLift and Rezum are similarly effective in improving urinary symptoms and function with no difference in surgical retreatment rates. The procedures differed in short-term clinical side-effect profile. Rezum patients reported more urinary retention, hematuria, and dysuria; UroLift patients had clot retention more frequently.
Source of Funding: None
Methods: Patients at an academic institution between 1/2017 and 1/2021 were screened, and those with preoperative prostate volume >30cc and =80cc were included. Patients with follow-up <30 days were excluded. Outcomes included changes in AUA symptom score (AUA-SS), Qmax, post void residual (PVR), surgical retreatment rate, changes in BPH medications use, postoperative complications, ER visits, and readmissions within 90 days.
Results: We identified 375 Rezum and 151 UroLift patients of which 191 Rezum (51%) and 88 UroLift (58%) patients met inclusion criteria. Median follow-up for Rezum and UroLift patients was 173 and 307 days, respectively. Compared to Rezum patients, UroLift patients were older (Rezum 67 ± 8 vs UroLift 69 ± 9 years, p=0.014) and had smaller prostates (Rezum 50.7 ± 13.5 vs UroLift 44.9 ± 12.4 cc, p<0.001). Preoperatively, UroLift patients had higher PVR (Rezum 93 ± 112 vs Urolift 156 ± 185 mL, p=0.028) and lower Qmax (Rezum 9.3 ± 5.1 vs UroLift 7.5 ± 4.6 mL/sec, p=0.004). After treatment, both Rezum and UroLift patients had significant, similar improvements in AUA-SS (Rezum -4.0 ± 6.8 vs. UroLift -5.2 ± 8.0 points, p=0.349) and PVR (Rezum -26.5 ± 91.8 vs UroLift -59.3 ± 150.3 mL, p=0.349). There was no significant improvement in Qmax (Table 1a). Both groups had decreased alpha-blocker use after treatment (Rezum 72.8% to 44.5%, UroLift 76.1% to 38.6%, both p<0.001) (Table 1b). In the postoperative 90-day period, Rezum patients experienced more hematuria, dysuria and retention, whereas UroLift patients more frequently had clot retention (Table 1c). There were no differences in 90-day ER visits, 90-day readmissions, or surgical retreatment rates (all p>0.05).
Conclusions: For patients with BPH, UroLift and Rezum are similarly effective in improving urinary symptoms and function with no difference in surgical retreatment rates. The procedures differed in short-term clinical side-effect profile. Rezum patients reported more urinary retention, hematuria, and dysuria; UroLift patients had clot retention more frequently.
Source of Funding: None

.jpg)
.jpg)