Back
Poster, Podium & Video Sessions
Podium
PD45: Benign Prostatic Hyperplasia: Surgical Therapy & New Technology IV
PD45-09: Long term outcome of a randomized clinical trial comparing thulium vaporization of the prostate versus monopolar TURP, the test of time.
Sunday, May 15, 2022
2:20 PM – 2:30 PM
Location: Room 252
Osama Ezzat*, Ahmed M. Elshal, Mahmoud Laymon, Ahmed El-Assmy, Ahmed Shoma, Mansoura, Egypt
Podium Presenter(s)
Introduction: To report the long term outcome of a randomized trial comparing high power thulium laser vaporization of the prostate (ThuVap) to Monopolar transurethral resection of the prostate (M-TURP) for treatment of mild to moderate benign prostatic obstruction (BPO).
Methods: Between May 2017 and December 2018, 110 patients (prostate size 30-80ml) were randomly allocated to ThuVap (54) and M-TURP (56). Patients were followed up at 1, 3, 6, 12 months then annually. In this analysis, retreatment rate will be our main concern. Patients with recurring LUTs will be examined by flexible cystoscopy and treatment will be planned accordingly. Urinary outcome measures (change in IPSS, Qmax, PVR, QOL score), percent PSA reduction, sexual function changes and late postoperative complications will be reported and compared between both groups.
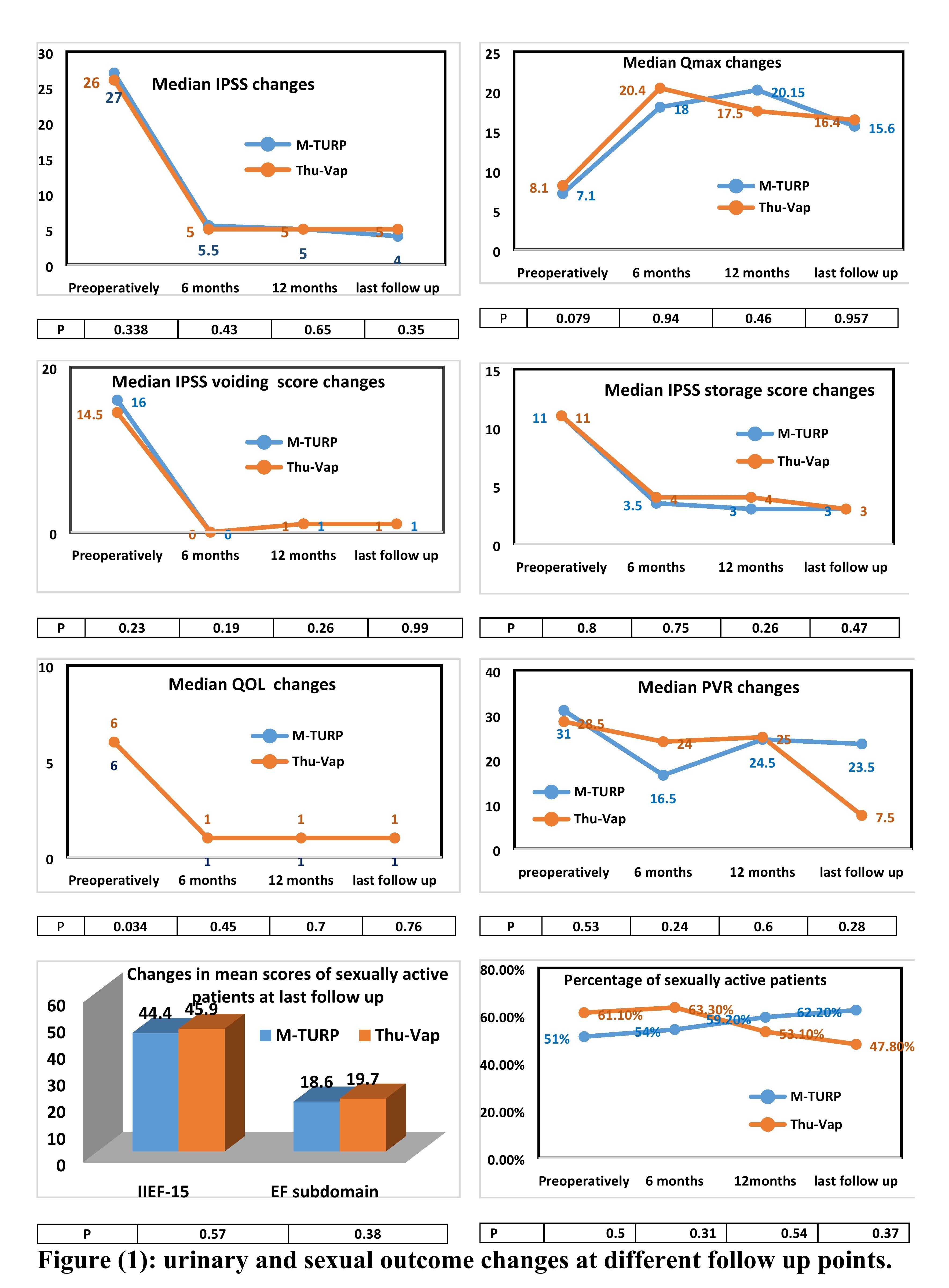
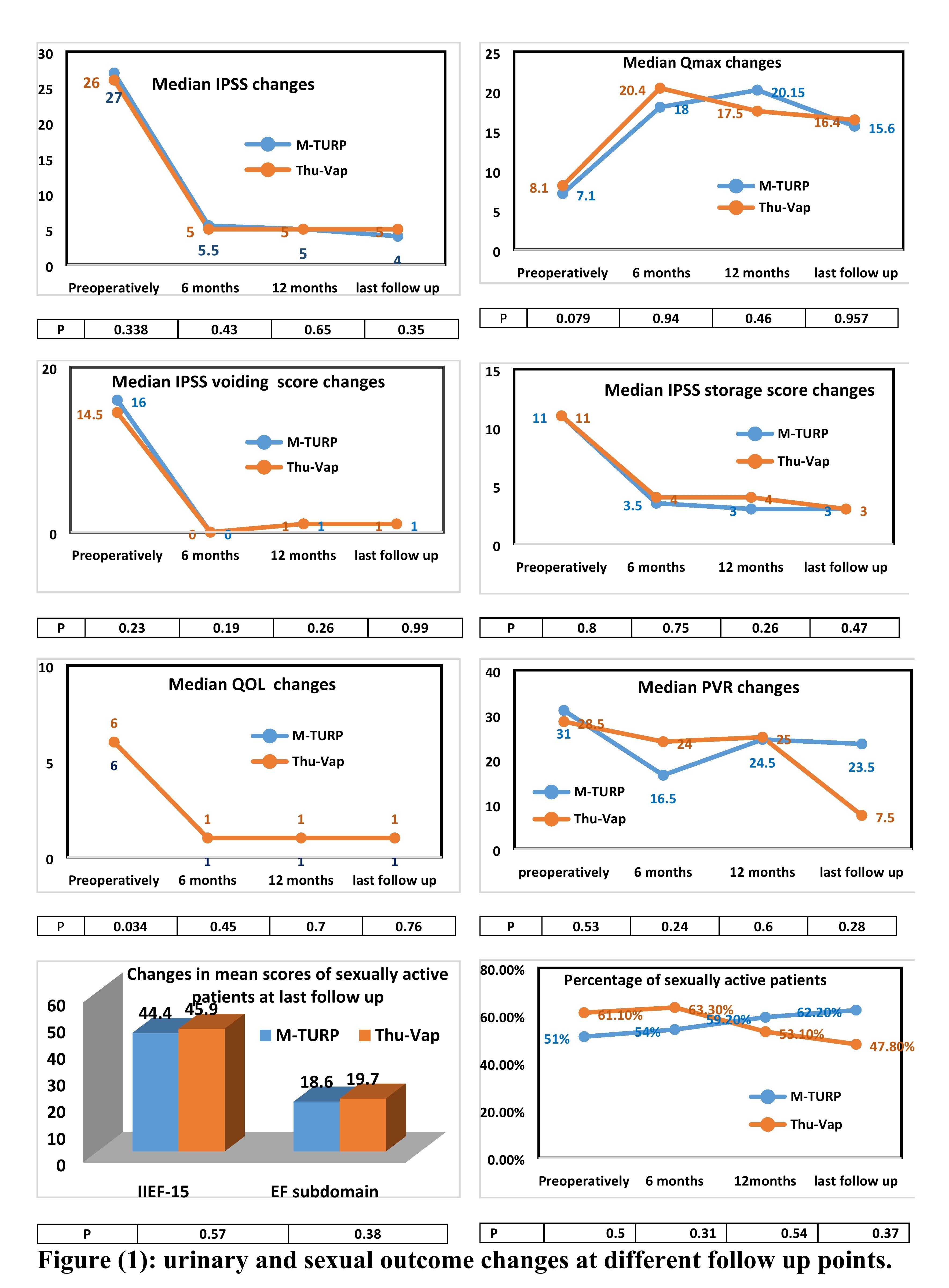
Results: After a median of 43.5 months (range 31- 52.6 months), 46 ThuVap and 45 M-TURP patients were evaluable with comparable significant improvement of urinary outcome measures from baseline at different follow up visits in both groups (P>0.05). (Figure1)
Recurrent LUTs due to Bladder Outlet Obstruction (BOO) was reported in 9 (19.5%) and 8 (17.8%) after ThuVap and M-TURP respectively (P=0.83). Reuse of alpha blockers was reported in 5 (10.9%) and 4 (8.9%) of ThuVap and M-TURP patients respectively (P=0.75). Reintervention was reported in 8.7% and 8.9% after ThuVap and M-TURP respectively (P=0.51) including prostate re-resection in 3 ThuVap and 2 M-TURP patients.
Median percent of PSA reduction at last follow-up was 59% and 57% in the ThuVap and M-TURP respectively (P=0.98).
Six (13%) ThuVap patients and single (2.2%) M-TURP patient reported stress urine incontinence (SUI) subjectively (P= 0.243). Using one-hour pad test, G0 (dry pad) was reported in 3 ThuVap patients and GI ( <10gm) SUI in the remaining patients.
Among sexually active men, there were no statistically significant difference at last follow up neither total IIEF-15 score nor its EF subdomain (P>0.05) (Figure1). Ejaculatory dysfunction was reported in 59.1% and 57.1% in ThuVap and M-TURP groups respectively (P= 1).
Conclusions: ThuVap could achieve durable control of LUTs secondary to small and moderate sized BPO comparable to M-TURP maintaining all safety advantages of laser.
Source of Funding: no funds received
Methods: Between May 2017 and December 2018, 110 patients (prostate size 30-80ml) were randomly allocated to ThuVap (54) and M-TURP (56). Patients were followed up at 1, 3, 6, 12 months then annually. In this analysis, retreatment rate will be our main concern. Patients with recurring LUTs will be examined by flexible cystoscopy and treatment will be planned accordingly. Urinary outcome measures (change in IPSS, Qmax, PVR, QOL score), percent PSA reduction, sexual function changes and late postoperative complications will be reported and compared between both groups.
Results: After a median of 43.5 months (range 31- 52.6 months), 46 ThuVap and 45 M-TURP patients were evaluable with comparable significant improvement of urinary outcome measures from baseline at different follow up visits in both groups (P>0.05). (Figure1)
Recurrent LUTs due to Bladder Outlet Obstruction (BOO) was reported in 9 (19.5%) and 8 (17.8%) after ThuVap and M-TURP respectively (P=0.83). Reuse of alpha blockers was reported in 5 (10.9%) and 4 (8.9%) of ThuVap and M-TURP patients respectively (P=0.75). Reintervention was reported in 8.7% and 8.9% after ThuVap and M-TURP respectively (P=0.51) including prostate re-resection in 3 ThuVap and 2 M-TURP patients.
Median percent of PSA reduction at last follow-up was 59% and 57% in the ThuVap and M-TURP respectively (P=0.98).
Six (13%) ThuVap patients and single (2.2%) M-TURP patient reported stress urine incontinence (SUI) subjectively (P= 0.243). Using one-hour pad test, G0 (dry pad) was reported in 3 ThuVap patients and GI ( <10gm) SUI in the remaining patients.
Among sexually active men, there were no statistically significant difference at last follow up neither total IIEF-15 score nor its EF subdomain (P>0.05) (Figure1). Ejaculatory dysfunction was reported in 59.1% and 57.1% in ThuVap and M-TURP groups respectively (P= 1).
Conclusions: ThuVap could achieve durable control of LUTs secondary to small and moderate sized BPO comparable to M-TURP maintaining all safety advantages of laser.
Source of Funding: no funds received

.jpg)
.jpg)
