Back
Poster, Podium & Video Sessions
Podium
PD47: Sexual Function/Dysfunction: Evaluation II
PD47-02: Association of Low Testosterone and Frailty Among Veterans Undergoing Cancer Surgery
Sunday, May 15, 2022
1:10 PM – 1:20 PM
Location: Room 245
Matthew Hudnall*, Neil Mistry, David Bentrem, Justin Dubin, Robert Brannigan, Joshua Halpern, Chicago, IL
- MH
Podium Presenter(s)
Introduction: Frailty is common among Veterans and is a key predictor of post-operative complication and mortality. The prevalence of low testosterone (T) and its relationship to frailty in the pre-operative cancer setting is not well established. We sought to characterize the prevalence of pre-operative low T in Veterans undergoing non-cardiac thoracic or abdominal-pelvic surgery for cancer and to determine the association between low T and frailty in these patients.
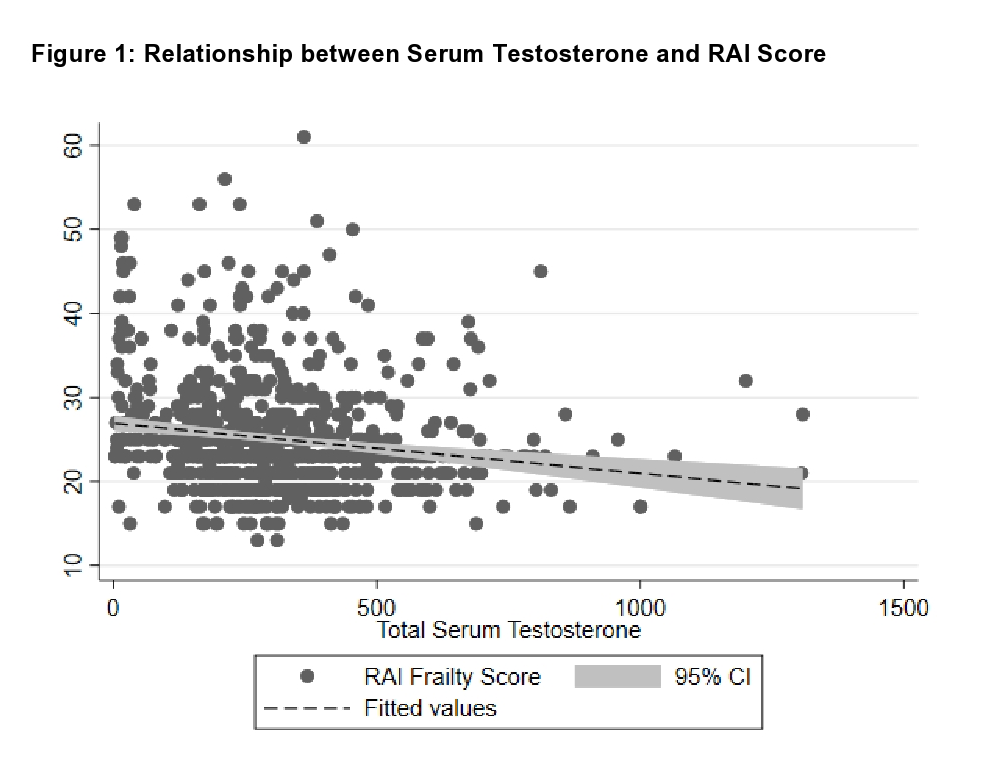
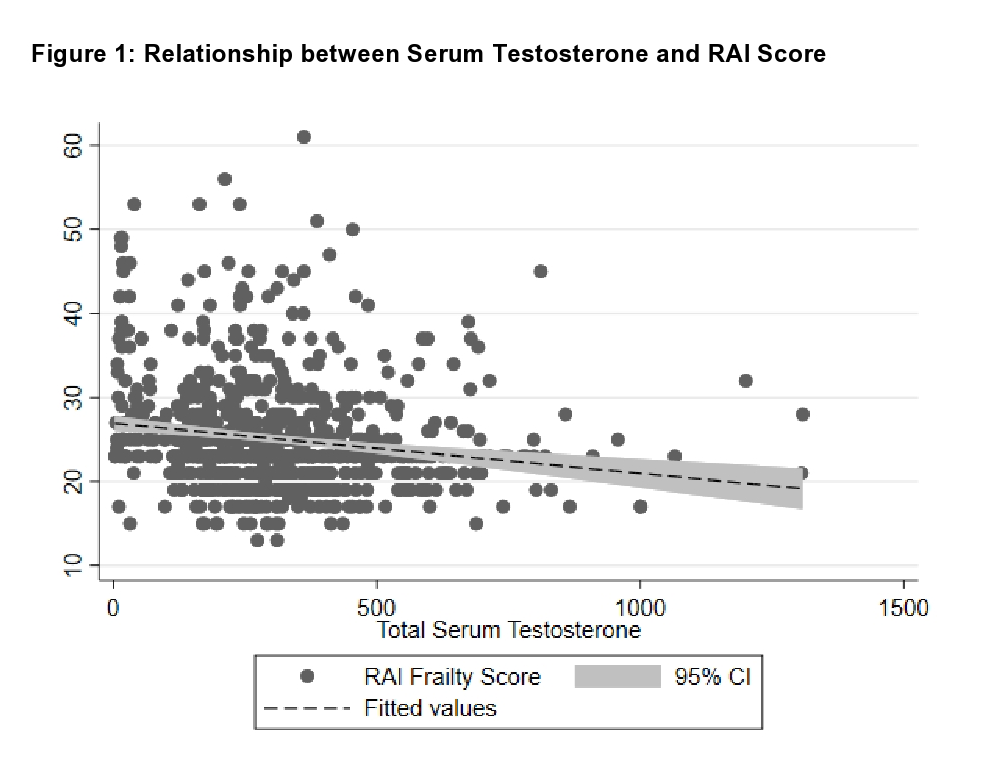
Methods: This retrospective cohort study included male patients age 40 and older in the Veteran Affairs Surgical Quality Improvement Program (VASQIP) undergoing thoracic or abdominal-pelvic surgery for cancer at Veterans Health Administration Hospitals between 2015 and 2018, with a total serum T measured within one year prior to the date of surgery. Low T was defined as < 300 ng/dL. Patients were categorized as robust, normal, frail, or very frail according to the Risk Analysis Index (RAI), a published frailty measure built upon data available in the VASQIP. The relationship between continuous RAI score and serum T was examined using linear regression. Ordered logistic regression adjusting for body mass index (BMI) and smoking status was used to evaluate the association between low T and RAI frailty category.
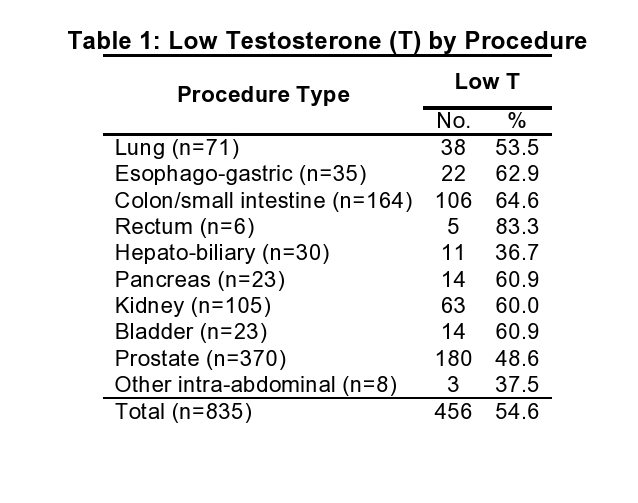
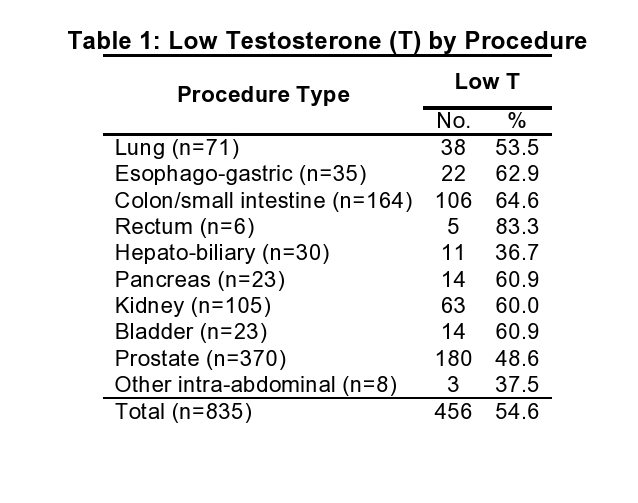
Results: Of 835 patients (mean age = 65.5), 54.6% had low T prior to surgery. Prevalence of low T varied by procedure, ranging from 37% to 83% (Table 1). 109 patients (13%) were considered frail and 37 (4.5%) were considered very frail. Increasing serum testosterone was associated with lower RAI score (Figure 1). The odds of being in a higher RAI frailty category was 1.68 times greater for patients with low T (95% confidence interval 1.26 – 2.25, p<0.001).
Conclusions: The prevalence of low T in Veterans undergoing non-cardiac thoracic or abdominal-pelvic cancer surgery is high and associated with increased frailty as measured by the RAI. Further exploration is necessary to determine whether serum testosterone improves the predictive capability of the RAI on post-operative outcomes.
Source of Funding: NA
Methods: This retrospective cohort study included male patients age 40 and older in the Veteran Affairs Surgical Quality Improvement Program (VASQIP) undergoing thoracic or abdominal-pelvic surgery for cancer at Veterans Health Administration Hospitals between 2015 and 2018, with a total serum T measured within one year prior to the date of surgery. Low T was defined as < 300 ng/dL. Patients were categorized as robust, normal, frail, or very frail according to the Risk Analysis Index (RAI), a published frailty measure built upon data available in the VASQIP. The relationship between continuous RAI score and serum T was examined using linear regression. Ordered logistic regression adjusting for body mass index (BMI) and smoking status was used to evaluate the association between low T and RAI frailty category.
Results: Of 835 patients (mean age = 65.5), 54.6% had low T prior to surgery. Prevalence of low T varied by procedure, ranging from 37% to 83% (Table 1). 109 patients (13%) were considered frail and 37 (4.5%) were considered very frail. Increasing serum testosterone was associated with lower RAI score (Figure 1). The odds of being in a higher RAI frailty category was 1.68 times greater for patients with low T (95% confidence interval 1.26 – 2.25, p<0.001).
Conclusions: The prevalence of low T in Veterans undergoing non-cardiac thoracic or abdominal-pelvic cancer surgery is high and associated with increased frailty as measured by the RAI. Further exploration is necessary to determine whether serum testosterone improves the predictive capability of the RAI on post-operative outcomes.
Source of Funding: NA

.jpg)
.jpg)