Back
Poster, Podium & Video Sessions
Podium
PD47: Sexual Function/Dysfunction: Evaluation II
PD47-08: Association of Sexual Dysfunction and Depression in Women Following Traumatic Pelvic Fracture
Sunday, May 15, 2022
2:10 PM – 2:20 PM
Location: Room 245
Helen Gambrah*, Niels Vass Johnsen, MD, MPH, Nashville, TN

Helen Gambrah, BA
Vanderbilt University School of Medicine
Podium Presenter(s)
Introduction: Women with traumatic pelvic fracture are at high risk for developing sexual dysfunction (SD) due to concomitant neurovascular damage. While SD is a well-known symptom of major depression, few studies discuss how newly acquired SD following trauma can lead to depressive mood. We hypothesized that the presence of SD after pelvic fracture increases risk for experiencing depressive symptoms.
Methods: Women treated for traumatic pelvic fractures at a single level 1 trauma center over a 5-year period were invited to participate in an online cross-sectional survey. Sexual function was evaluated using the Female Sexual Function Index (FSFI), with a score of less than 26.55 signifying SD. Depression was assessed using the 8-item patient health questionnaire (PHQ-8), with major depression defined as a PHQ-8 score = 10. Inverse probability weighting was utilized to adjust for subject nonresponse. Multivariate regression was performed to assess the impact of SD on patient-reported depression.
Results: 98 of the 780 potential subjects responded to the survey (12.6%). Responders had a mean age at the time of injury of 42.2 years (SD 22.4) and median time since injury of 45 months (IQR 30.0, 57.4). After weighting, 72.2% of women reported SD based on FSFI, with a median score of 10.4 (IQR 4.3, 19.9) in women with SD.
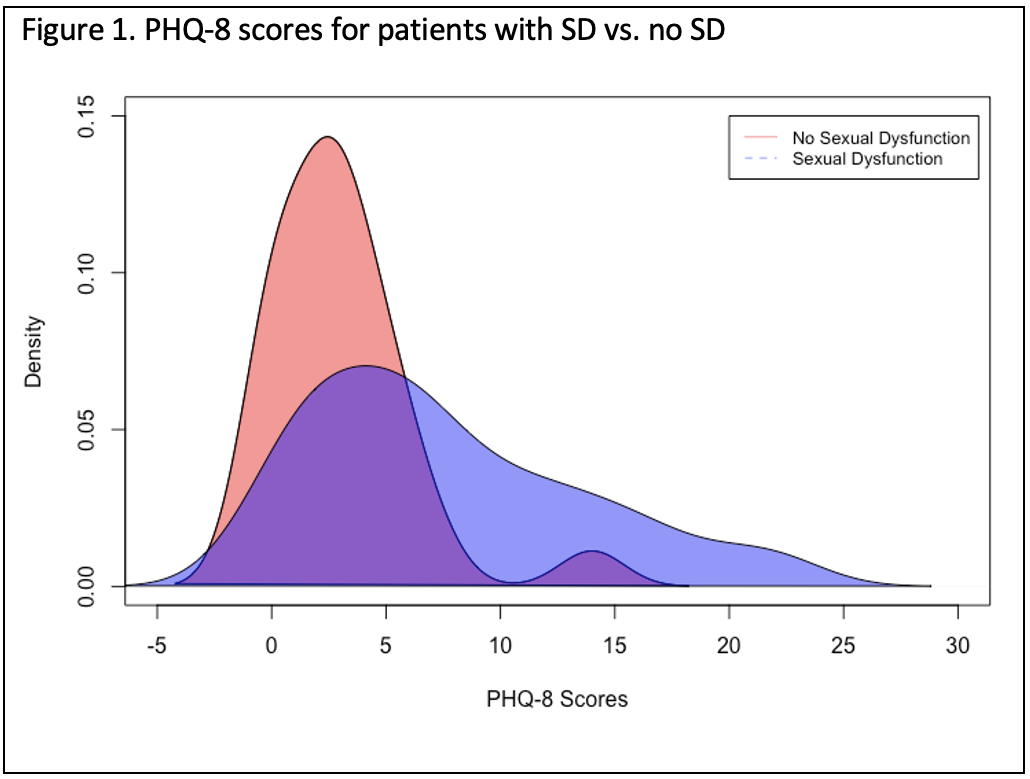
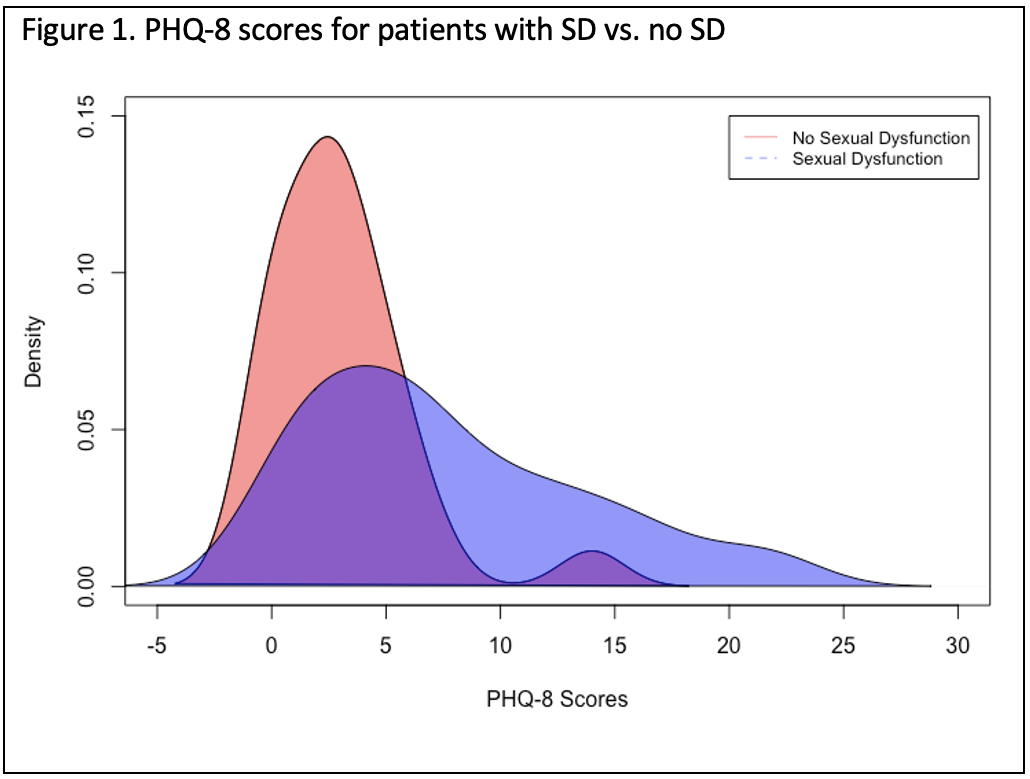
Women reporting SD had significantly higher PHQ-8 scores with a median PHQ-8 score of 6 (IQR 2, 11) relative to those without SD who had a median score of 2 (IQR 0,2) (p <0.001). On multivariate linear regression, presence of SD was significantly associated with higher PHQ-8 scores (ß = 4.91, 95% CI 2.8 – 7.0, p<0.001) (Figure 1). After dichotomizing PHQ-8 scores to major depression and no depression, multivariate logistic regression demonstrated that the presence of SD was an independent predictor of major depression (OR 1.37, 95% CI 1.18 – 1.59, p<0.001).
Conclusions: SD is prevalent in women following traumatic pelvic fracture. Women with SD reported feeling depressive symptoms more frequently than those without SD and were more likely to report symptoms of major depression. These results suggest that women with persistent SD following traumatic pelvic fracture may be at greater risk for developing depression, emphasizing the need for both routine sexual health and depression screening in the post-injury setting.
Source of Funding: None
Methods: Women treated for traumatic pelvic fractures at a single level 1 trauma center over a 5-year period were invited to participate in an online cross-sectional survey. Sexual function was evaluated using the Female Sexual Function Index (FSFI), with a score of less than 26.55 signifying SD. Depression was assessed using the 8-item patient health questionnaire (PHQ-8), with major depression defined as a PHQ-8 score = 10. Inverse probability weighting was utilized to adjust for subject nonresponse. Multivariate regression was performed to assess the impact of SD on patient-reported depression.
Results: 98 of the 780 potential subjects responded to the survey (12.6%). Responders had a mean age at the time of injury of 42.2 years (SD 22.4) and median time since injury of 45 months (IQR 30.0, 57.4). After weighting, 72.2% of women reported SD based on FSFI, with a median score of 10.4 (IQR 4.3, 19.9) in women with SD.
Women reporting SD had significantly higher PHQ-8 scores with a median PHQ-8 score of 6 (IQR 2, 11) relative to those without SD who had a median score of 2 (IQR 0,2) (p <0.001). On multivariate linear regression, presence of SD was significantly associated with higher PHQ-8 scores (ß = 4.91, 95% CI 2.8 – 7.0, p<0.001) (Figure 1). After dichotomizing PHQ-8 scores to major depression and no depression, multivariate logistic regression demonstrated that the presence of SD was an independent predictor of major depression (OR 1.37, 95% CI 1.18 – 1.59, p<0.001).
Conclusions: SD is prevalent in women following traumatic pelvic fracture. Women with SD reported feeling depressive symptoms more frequently than those without SD and were more likely to report symptoms of major depression. These results suggest that women with persistent SD following traumatic pelvic fracture may be at greater risk for developing depression, emphasizing the need for both routine sexual health and depression screening in the post-injury setting.
Source of Funding: None

.jpg)
.jpg)