Back
Poster, Podium & Video Sessions
Podium
PD51: Penile & Testicular Cancer II
PD51-01: Contemporary Surgical Outcomes of Retroperitoneal Lymph Node Dissection From the SEMS Trial
Sunday, May 15, 2022
3:30 PM – 3:40 PM
Location: Room 245
Brian Hu*, Loma Linda, CA, Muhannad Alsyouf, Los Angeles, CA, Clint Cary, Timothy A. Masterson, Lawrence Einhorn, Indianapolis, IN, Stephen A. Boorjian, Rochester, MN, Christian K. Kollmannsberger, Vancouver, Canada, Anne K. Schuckman, Los Angeles, CA, Alan So, Peter C. Black, Vancouver, Canada, Aditya Bagrodia, Dallas, TX, Eila C. Skinner, Palo Alto, CA, Mehrdad Alemozaffar, Atlanta, GA, Timothy C. Brand, Tacoma, WA, Scott E. Eggener, Chicago, IL, Phillip M. Pierorazio, Baltimore, MD, Kelly Lynn Stratton, Oklahoma , OK, Lucia Nappi, Vancouver, Canada, Craig R. Nichols, Seattle, WA, Siamak Daneshmand, Los Angeles, CA
- BH
Podium Presenter(s)
Introduction: The literature on peri-operative outcomes and long-term complications of retroperitoneal lymph node dissection (RPLND) is largely retrospective, single institution and historical. The SEMS trial established primary RPLND as an option for treating seminoma with isolated retroperitoneal lymphadenopathy. We describe this multi-institutional trial’s surgical outcomes.
Methods: A review of the phase II, prospective clinical trial data of patients with treatment naïve testicular seminoma and isolated retroperitoneal lymphadenopathy (1-3 cm) was performed. Patients underwent open RPLND and were seen for a post-operative visit within 30 days of surgery and then at routine intervals. History, physical, laboratory and radiographic evaluation were performed at each visit. Complications within 30 days were classified using the Clavien-Dindo system. Nerve-sparing approach was determined by operative reports and confirmed by an independent review of intra-operative photos.
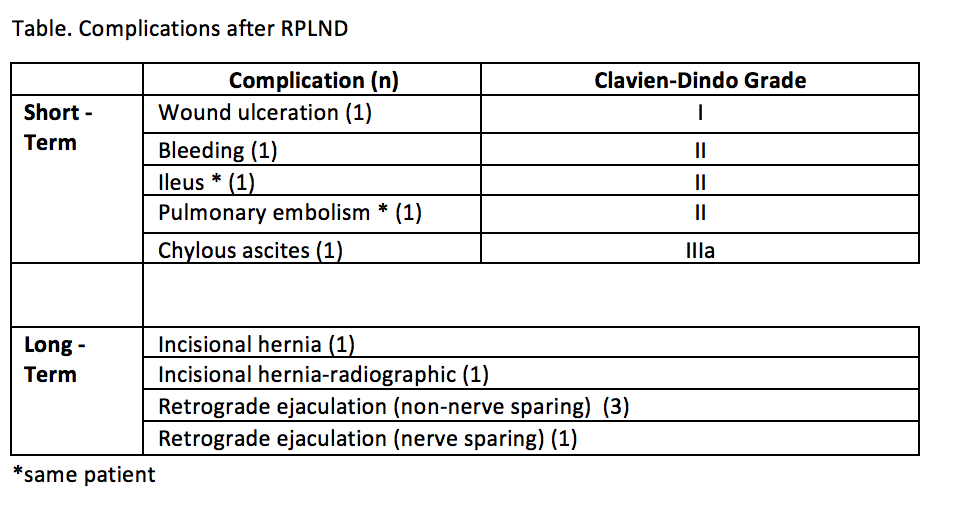
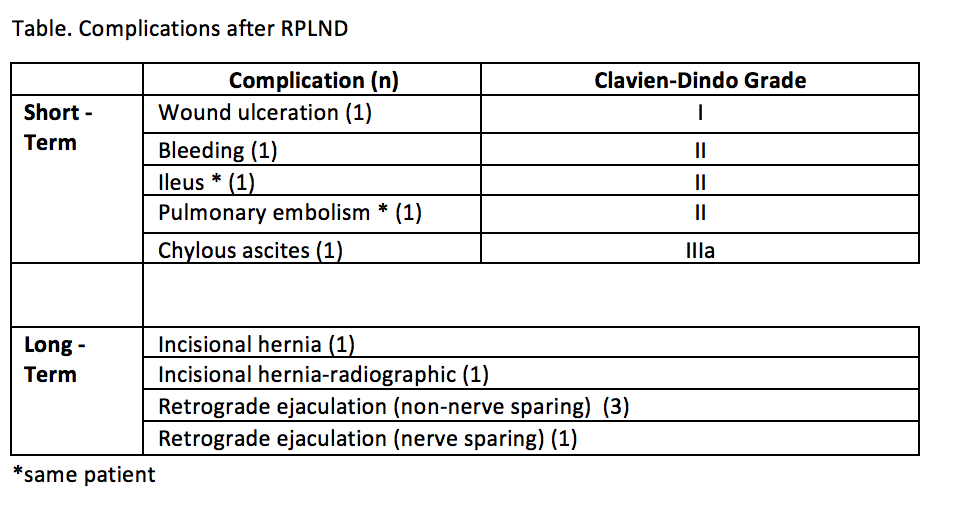
Results: The study consisted of 55 patients who were enrolled at 12 institutions with 19 different surgeons. RPLND was performed via both transperitoneal (n=40) and midline extraperitoneal (n=15) techniques with a median duration of surgery of 233 (IQR 178-313) minutes. The template of dissection was bilateral (n=19), left modified (n=25), and right modified (n=11). Nerve-sparing within the template was performed in 48 (87%) patients. Median blood loss was 150 (IQR 100-300) ml and no patients required intraoperative blood transfusion. Median length of stay was 3 (IQR 2-4) days and a median follow-up of 33 (IQR 27-40) months. Four (7%) patients experienced five short-term complication: 1 had Clavien-Dindo grade I, 3 had grade II, and 1 had grade IIIa. Six (11%) patients experienced a long-term complication (Table), including incisional hernia in 2 patients (one was asymptomatic and only seen radiographically) and retrograde ejaculation in 3 patients. Antegrade ejaculation was preserved in 98% of patients who underwent nerve-sparing surgery.
Conclusions: In a contemporary prospective surgical trial across multiple institutions, primary RPLND is associated with low rates of perioperative morbidity and complications.
Source of Funding: Think Different Foundation
Methods: A review of the phase II, prospective clinical trial data of patients with treatment naïve testicular seminoma and isolated retroperitoneal lymphadenopathy (1-3 cm) was performed. Patients underwent open RPLND and were seen for a post-operative visit within 30 days of surgery and then at routine intervals. History, physical, laboratory and radiographic evaluation were performed at each visit. Complications within 30 days were classified using the Clavien-Dindo system. Nerve-sparing approach was determined by operative reports and confirmed by an independent review of intra-operative photos.
Results: The study consisted of 55 patients who were enrolled at 12 institutions with 19 different surgeons. RPLND was performed via both transperitoneal (n=40) and midline extraperitoneal (n=15) techniques with a median duration of surgery of 233 (IQR 178-313) minutes. The template of dissection was bilateral (n=19), left modified (n=25), and right modified (n=11). Nerve-sparing within the template was performed in 48 (87%) patients. Median blood loss was 150 (IQR 100-300) ml and no patients required intraoperative blood transfusion. Median length of stay was 3 (IQR 2-4) days and a median follow-up of 33 (IQR 27-40) months. Four (7%) patients experienced five short-term complication: 1 had Clavien-Dindo grade I, 3 had grade II, and 1 had grade IIIa. Six (11%) patients experienced a long-term complication (Table), including incisional hernia in 2 patients (one was asymptomatic and only seen radiographically) and retrograde ejaculation in 3 patients. Antegrade ejaculation was preserved in 98% of patients who underwent nerve-sparing surgery.
Conclusions: In a contemporary prospective surgical trial across multiple institutions, primary RPLND is associated with low rates of perioperative morbidity and complications.
Source of Funding: Think Different Foundation

.jpg)
.jpg)