Back
Poster, Podium & Video Sessions
Podium
PD51: Penile & Testicular Cancer II
PD51-05: Feasibility of omitting CT pelvis in patients with stage I germ cell tumor (GCT) on active surveillance: A multi-institutional study
Sunday, May 15, 2022
4:10 PM – 4:20 PM
Location: Room 245
Hamed Ahmadi*, Minneapolis, MN, Tarik Benidir, Cleveland, OH, Ragheed Saoud, New Jersey , NJ, Lynn Anson-Cartwright, Martin O’Malley, Toronto , Canada, Scott E Eggener, Chicago , IL, Robert J Hamilton, Toronto , Canada, Siamak Daneshmand, Los Angeles, CA
- HA
Podium Presenter(s)
Introduction: Surveillance for stage I GCTs typically includes periodic imaging of chest, abdomen and pelvis. Every effort should be made to minimize radiation exposure in this young patient population. We report the results of our multi-institutional study assessing the effect of omitting CT pelvis on detection of recurrent disease.
Methods: Using data from three major referral centers for GCT (University of Southern California, University of Toronto, and University of Chicago), all patients with stage I GCT who experienced recurrence on active surveillance were selected. Clinicodemographic information including recurrence pattern (tumor marker (TM), imaging, physical exam (PE), or a combination of these) were collected. Bifurcation of the common iliac arteries was defined as the anatomic landmark between CT abdomen and CT pelvis. The location of recurrent nodal disease was determined accordingly.
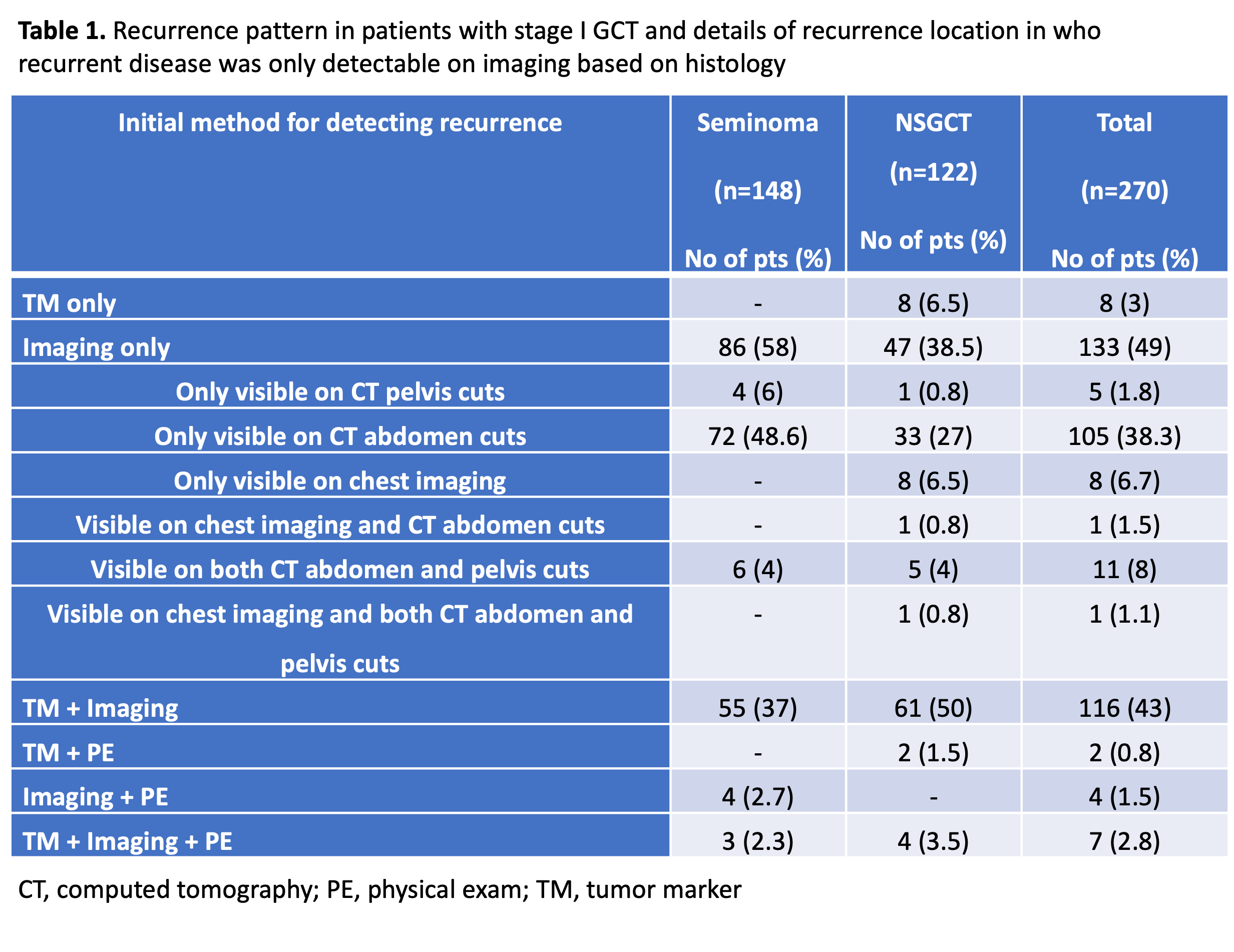
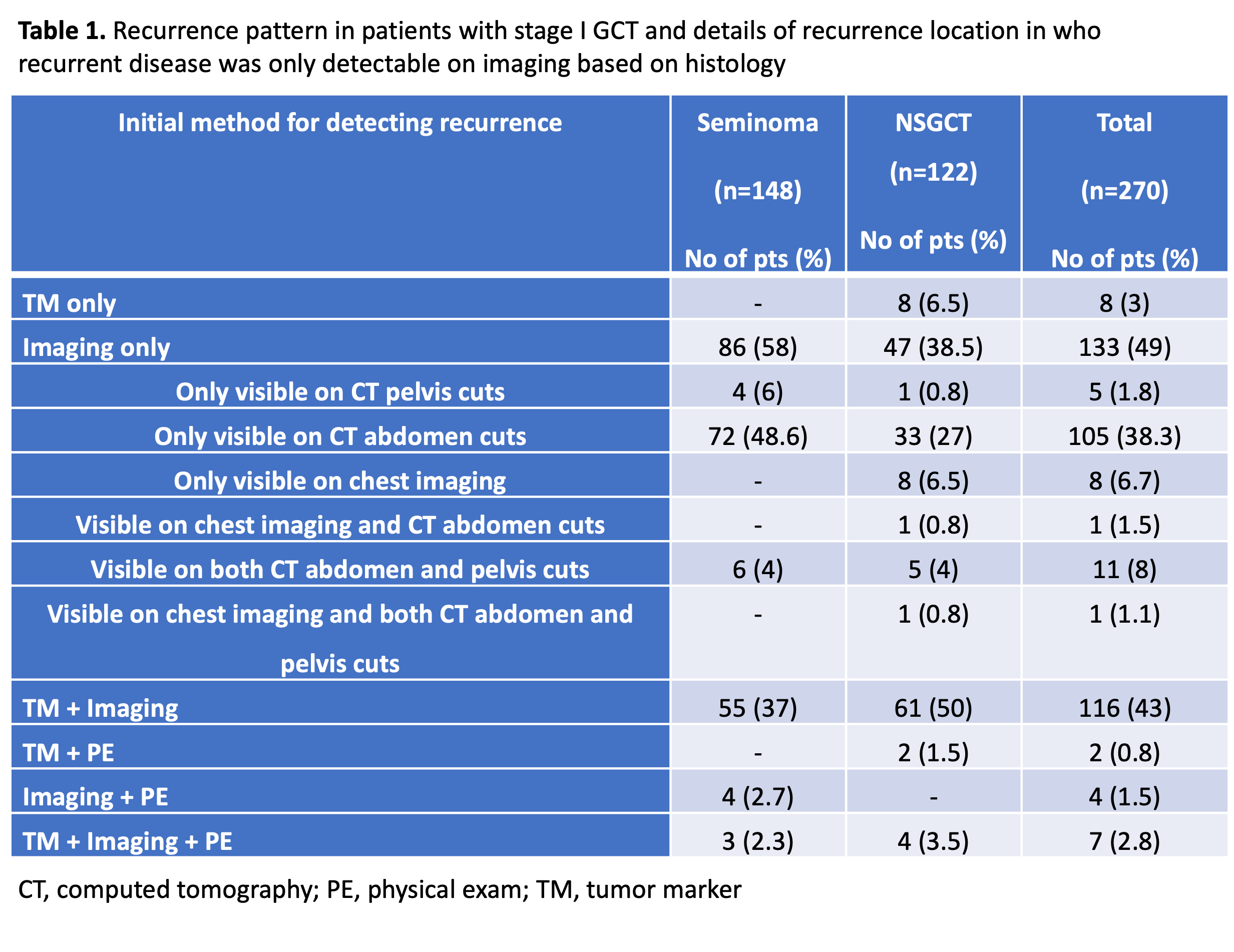
Results: A total of 270 who had disease recurrence were included in the study. 122 (45%) patients had non-seminomatous GCT (NSGCT). 17 (6%) patients had a history of cryptorchidism and 38 (14%) had a history of scrotal/inguinal surgery. The median time to recurrence was 16 months (IQR 8 – 27 months) for seminoma and 6 months (IQR 4 – 13 months) for NSGCT. The most common modality for initial detection of recurrence was imaging only (49%) followed by combination of TM and imaging (43%). A total of 43/270 (16%) patients had pelvic/inguinal nodal recurrence. There was significantly higher percentage of prior hernia repair in these patients compared to the ones with no pelvic/inguinal nodal disease (19% vs 2.5%; p=0.01). Pelvic/inguinal nodal disease was detectable only by imaging in 16/270 (6%) patients. However, in 11/16 (69%) patients, pelvic/inguinal nodal disease was either visible on CT abdomen cuts or there was simultaneous retroperitoneal nodal disease. Overall, only 5/270 (1.8%) patients (4 seminoma, 1 non-seminoma) had pelvic/inguinal recurrence only detectable on CT pelvis.
Conclusions: CT scan of the abdomen only in combination with chest imaging, TMS and PE detect vast majority of recurrences in this multi-institutional series. CT pelvis can be safely omitted during AS of stage I GCT. Future modification in guidelines for AS protocols of stage I GCT may be warranted with further mounting evidence.
Source of Funding: None
Methods: Using data from three major referral centers for GCT (University of Southern California, University of Toronto, and University of Chicago), all patients with stage I GCT who experienced recurrence on active surveillance were selected. Clinicodemographic information including recurrence pattern (tumor marker (TM), imaging, physical exam (PE), or a combination of these) were collected. Bifurcation of the common iliac arteries was defined as the anatomic landmark between CT abdomen and CT pelvis. The location of recurrent nodal disease was determined accordingly.
Results: A total of 270 who had disease recurrence were included in the study. 122 (45%) patients had non-seminomatous GCT (NSGCT). 17 (6%) patients had a history of cryptorchidism and 38 (14%) had a history of scrotal/inguinal surgery. The median time to recurrence was 16 months (IQR 8 – 27 months) for seminoma and 6 months (IQR 4 – 13 months) for NSGCT. The most common modality for initial detection of recurrence was imaging only (49%) followed by combination of TM and imaging (43%). A total of 43/270 (16%) patients had pelvic/inguinal nodal recurrence. There was significantly higher percentage of prior hernia repair in these patients compared to the ones with no pelvic/inguinal nodal disease (19% vs 2.5%; p=0.01). Pelvic/inguinal nodal disease was detectable only by imaging in 16/270 (6%) patients. However, in 11/16 (69%) patients, pelvic/inguinal nodal disease was either visible on CT abdomen cuts or there was simultaneous retroperitoneal nodal disease. Overall, only 5/270 (1.8%) patients (4 seminoma, 1 non-seminoma) had pelvic/inguinal recurrence only detectable on CT pelvis.
Conclusions: CT scan of the abdomen only in combination with chest imaging, TMS and PE detect vast majority of recurrences in this multi-institutional series. CT pelvis can be safely omitted during AS of stage I GCT. Future modification in guidelines for AS protocols of stage I GCT may be warranted with further mounting evidence.
Source of Funding: None

.jpg)
.jpg)