Back
Poster, Podium & Video Sessions
Podium
PD51: Penile & Testicular Cancer II
PD51-09: Survival in N3 penile cancer: does pelvic lymphadenopathy predict a worse prognosis than inguinal extra-nodal extension?
Sunday, May 15, 2022
4:50 PM – 5:00 PM
Location: Room 245
James A Churchill*, Ashwin Sachdeva, Allaudin Issa, Craig Jones, Fowz Azhar, Ikenna Aneke, Noel W Clarke, Maurice W Lau, Vijay K Sangar, Arie S Parnham, Manchester, United Kingdom

James Churchill, MBBS
Specialty Doctor in Urology
The Christie NHS Foundation Trust
Podium Presenter(s)
Introduction: Penile squamous cell cancer (PSCC) with lymph node (LN) metastatic disease is associated with poor survival. Current TNM classification systems define clinical N3 (cN3) stage as the presence of a fixed inguinal LN metastasis or pelvic lymphadenopathy (PLN), and pathologic N3 (pN3) stage as metastasis in pelvic LN and/or extra-nodal extension (ENE) at any regional LN metastasis. We hypothesised a worse overall survival for patients with PLN present on cross-sectional imaging compared to those with ENE present or absent in inguinal lymph node metastases (iENE) and PLN absent, with the aim of differentiating the N3 stage to more accurately select patients likely to benefit from adjuvant or palliative treatment. Audit approval was obtained from the host clinical governance committee.
Methods: We analysed retrospective data for patients treated at a single UK tertiary referral centre between 2003 and 2021 with PSCC and suspicion of nodal disease (cN+) at diagnosis. We excluded patients with extra-pelvic LN or distant metastatic disease at diagnosis and those without available CT, MRI or FDG-PET imaging of the abdomen and pelvis within 6 months of definitive primary (penile) treatment. We compared the primary outcome of overall survival of patients with iENE absent and PLN absent (iENE-PLN-) to patients with iENE present and PLN absent (iENE+PLN-) and to patients with PLN present on cross-sectional imaging (PLN+).
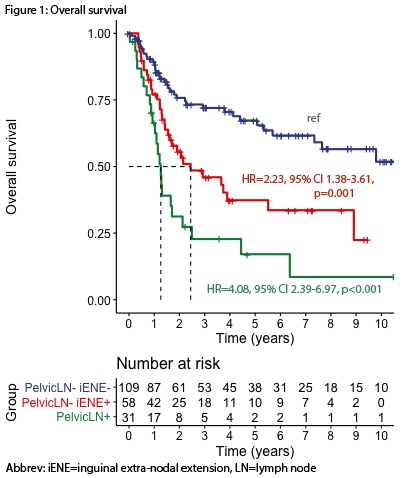
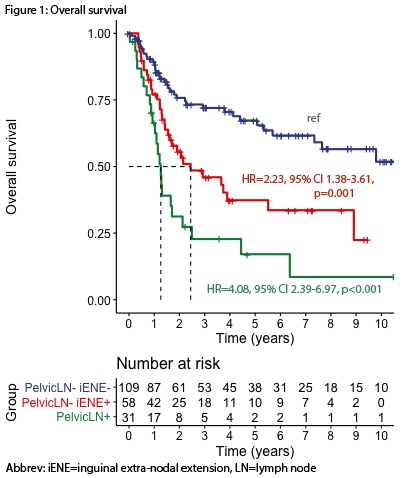
Results: 199 patients met inclusion criteria, of which 110 were categorised as iENE-PLN-, 58 as iENE+PLN- and 31 as PLN+. Baseline characteristics of age, primary tumour stage and grade were similar across the three groups. Univariate Cox regression analysis demonstrated an increased risk of death in the iENE+PLN- group (HR=2.23, 95% CI 1.38-3.61, p=0.001) and substantially increased risk of death in the PLN+ group (HR=4.08, 95% CI 2.39-6.97, p<0.001) compared to the iENE-PLN- group (figure 1).
Conclusions: In patients with PSCC and clinical suspicion of LN metastases, presence of iENE confers a 2.23x risk and presence of PLN confers a 4.08x risk of death, compared with absence of both risk factors. Refinement of the current TNM classification system is warranted to improve prognostic accuracy in LN metastatic staging.
Source of Funding: None
Methods: We analysed retrospective data for patients treated at a single UK tertiary referral centre between 2003 and 2021 with PSCC and suspicion of nodal disease (cN+) at diagnosis. We excluded patients with extra-pelvic LN or distant metastatic disease at diagnosis and those without available CT, MRI or FDG-PET imaging of the abdomen and pelvis within 6 months of definitive primary (penile) treatment. We compared the primary outcome of overall survival of patients with iENE absent and PLN absent (iENE-PLN-) to patients with iENE present and PLN absent (iENE+PLN-) and to patients with PLN present on cross-sectional imaging (PLN+).
Results: 199 patients met inclusion criteria, of which 110 were categorised as iENE-PLN-, 58 as iENE+PLN- and 31 as PLN+. Baseline characteristics of age, primary tumour stage and grade were similar across the three groups. Univariate Cox regression analysis demonstrated an increased risk of death in the iENE+PLN- group (HR=2.23, 95% CI 1.38-3.61, p=0.001) and substantially increased risk of death in the PLN+ group (HR=4.08, 95% CI 2.39-6.97, p<0.001) compared to the iENE-PLN- group (figure 1).
Conclusions: In patients with PSCC and clinical suspicion of LN metastases, presence of iENE confers a 2.23x risk and presence of PLN confers a 4.08x risk of death, compared with absence of both risk factors. Refinement of the current TNM classification system is warranted to improve prognostic accuracy in LN metastatic staging.
Source of Funding: None

.jpg)
.jpg)