Back
Poster, Podium & Video Sessions
Podium
PD51: Penile & Testicular Cancer II
PD51-11: Concomitant vs Staged Lymphadenectomy in Clinically Node-Positive Penile Squamous Cell Carcinoma: Recurrence Patterns and Survival Outcomes
Sunday, May 15, 2022
5:10 PM – 5:20 PM
Location: Room 245
Heather Huelster*, Tampa, FL, Marco Bandini, Milan, Italy, Oscar Brouwer, Amsterdam, Netherlands, Maarten Albersen, Eduard Roussel, Leuven, Belgium, Hielke de Vries, Amsterdam, Netherlands, Juan Chipollini, Mounsif Azizi, Tampa, FL, Yao Zhu, Ding-Wei Ye, Shanghai, China, People's Republic of, Antonio Ornellas, Rio de Janeiro, Brazil, Mario Catanzaro, Laura Marandino, Milan, Italy, Oliver Hakenberg, Rostock, Germany, Axel Heidenreich, Friederike Haidl, Köln, Germany, Nick Watkin, Michael Ager, London, United Kingdom, Mohamed Ahmed, Jeffrey Karnes, Rochester, MN, Alberto Briganti, Roberto Salvioni, Francesco Montorsi, Andrea Necchi, Milan, Italy, Philippe Spiess, Tampa, FL

Heather L. Huelster, MD
H Lee Moffitt Cancer Center & Research Institute
Podium Presenter(s)
Introduction: Inguinal lymph node dissection (LND) within 3 months of surgery on the primary tumor in penile cancer has been associated with longer recurrence-free (RFS) and cancer-specific survival (CSS). However, the effect of lymphadenectomy performed concurrently at the time of management of the primary lesion on oncologic outcomes in clinically node-positive penile squamous cell carcinoma (cN+ pSCC) remains unknown.
Methods: An international, multicenter cohort of 966 penile cancer cases from 1964 to 2019 from the USA, Europe, Brazil, and China was queried for pSCC management after the year 2000, cN+, and performance of penile surgery and ILND.
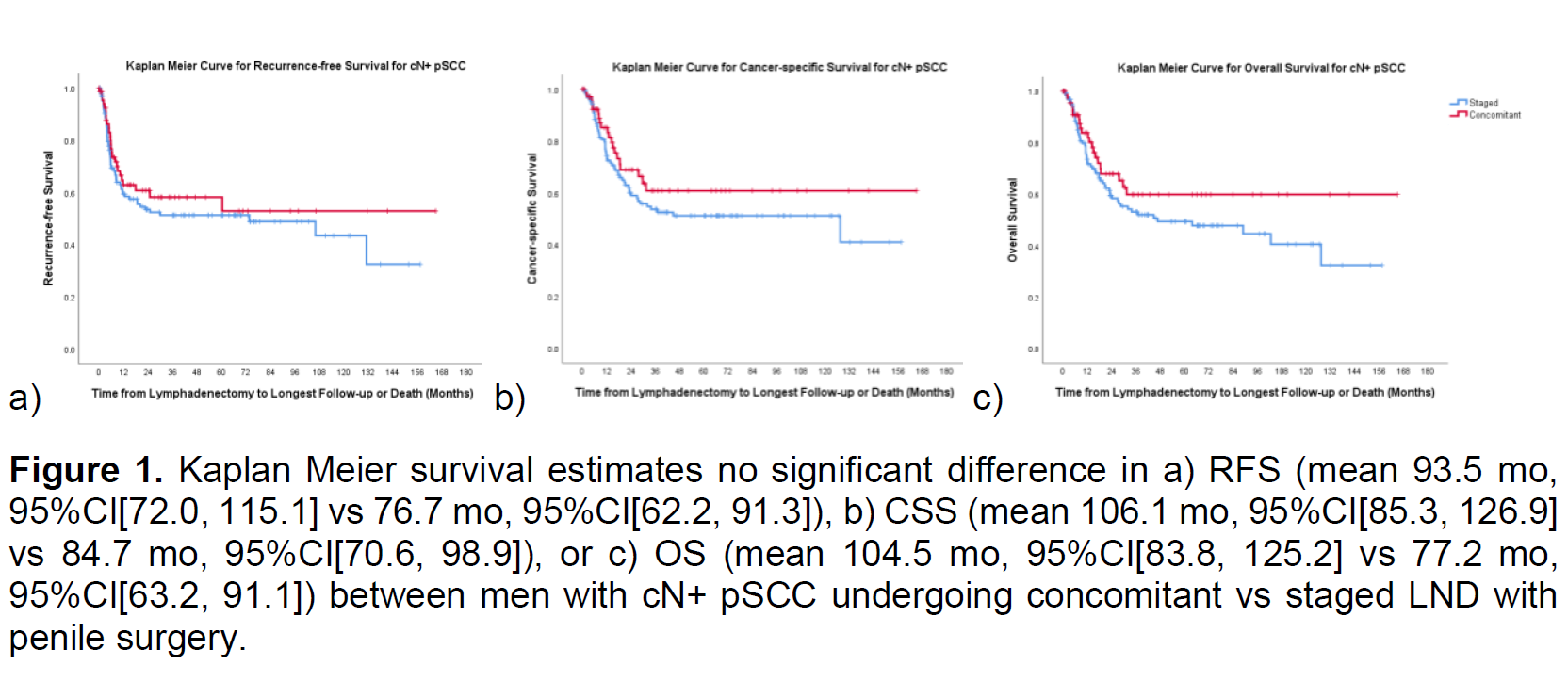
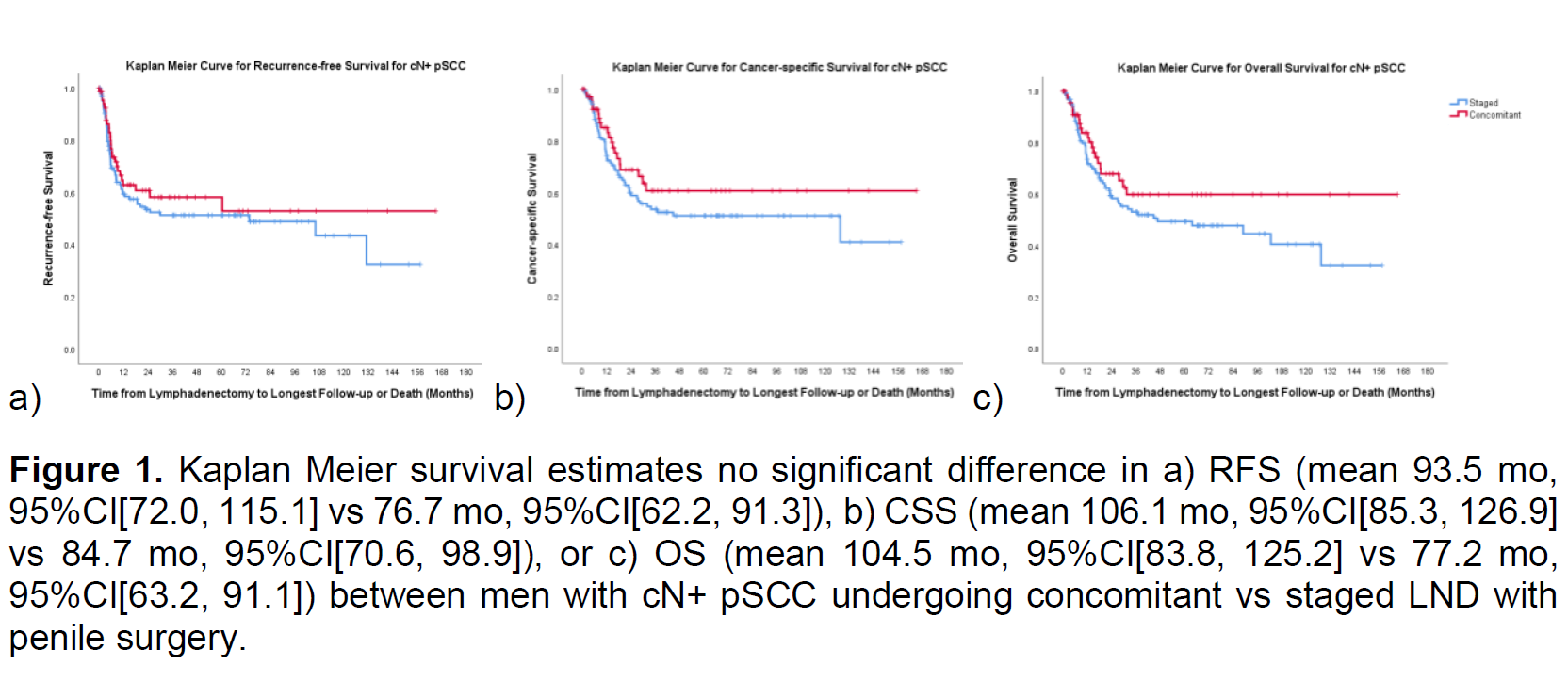
Cohorts were stratified as concomitant if LND and primary tumor surgery occurred on the same date or staged when LND was performed after penile surgery. Primary outcome was pSCC recurrence. Kaplan Meier survival estimates were compared with Mantel Cox log-rank tests. Multivariable Cox proportional hazard regression modeling determined associations with RFS, CSS, and overall survival (OS).
Results: Of 247 contemporary men with cN+ pSCC, 25 (9.2%) underwent LND prior to management of the primary tumor, 91 (33.5%) underwent concomitant LND, and 156 (57.3%) had LND performed after penile surgery. Recurrences developed in 128 (47.1%) of all patients, and men undergoing staged LND had a higher recurrence rate (49.4% vs 35.2%, p=0.03) than those with concomitant LND. Distant metastases were more common (38.3%) than inguinal (30.5%), penile (7.0%), or pelvic (6.3%) recurrence with no significant differences between concomitant and staged LND groups.
There were no significant differences in RFS, CSS, or OS between management strategies (Fig 1). Multivariable analysis adjusting for smoking, performance status, and pT stage demonstrated no survival differences between management strategies (p=0.23 and 0.11) but showed that younger age (p=0.08 and 0.05) and neoadjuvant chemotherapy administration (p=0.006 and 0.01) correlated with longer RFS and OS in men with cN+ pSCC undergoing penile tumor surgery and LND.
Conclusions: Inguinal lymph node dissection performed concurrently with penile surgery for clinically node-positive pSCC is associated with a lower recurrence rate but did not affect RFS, CSS, or OS compared to staged LND.
Source of Funding: None
Methods: An international, multicenter cohort of 966 penile cancer cases from 1964 to 2019 from the USA, Europe, Brazil, and China was queried for pSCC management after the year 2000, cN+, and performance of penile surgery and ILND.
Cohorts were stratified as concomitant if LND and primary tumor surgery occurred on the same date or staged when LND was performed after penile surgery. Primary outcome was pSCC recurrence. Kaplan Meier survival estimates were compared with Mantel Cox log-rank tests. Multivariable Cox proportional hazard regression modeling determined associations with RFS, CSS, and overall survival (OS).
Results: Of 247 contemporary men with cN+ pSCC, 25 (9.2%) underwent LND prior to management of the primary tumor, 91 (33.5%) underwent concomitant LND, and 156 (57.3%) had LND performed after penile surgery. Recurrences developed in 128 (47.1%) of all patients, and men undergoing staged LND had a higher recurrence rate (49.4% vs 35.2%, p=0.03) than those with concomitant LND. Distant metastases were more common (38.3%) than inguinal (30.5%), penile (7.0%), or pelvic (6.3%) recurrence with no significant differences between concomitant and staged LND groups.
There were no significant differences in RFS, CSS, or OS between management strategies (Fig 1). Multivariable analysis adjusting for smoking, performance status, and pT stage demonstrated no survival differences between management strategies (p=0.23 and 0.11) but showed that younger age (p=0.08 and 0.05) and neoadjuvant chemotherapy administration (p=0.006 and 0.01) correlated with longer RFS and OS in men with cN+ pSCC undergoing penile tumor surgery and LND.
Conclusions: Inguinal lymph node dissection performed concurrently with penile surgery for clinically node-positive pSCC is associated with a lower recurrence rate but did not affect RFS, CSS, or OS compared to staged LND.
Source of Funding: None

.jpg)
.jpg)