Back
Poster, Podium & Video Sessions
Podium
PD54: Prostate Cancer: Localized: Surgical Therapy III
PD54-01: Redefining Opioid Use After Prostatectomy: Results from the Implementation of a Statewide Opioid-Free Pain Optimization Pathway
Monday, May 16, 2022
7:00 AM – 7:10 AM
Location: Room 245
Udit Singhal*, Ji Qi, Ann Arbor, MI, Kevin Ginsberg, Detroit, MI, Alice Semerjian, Ann Arbor, MI, Thomas Maatman, Grand Rapids, MI, John Dibianco, Todd M. Morgan, Jeffrey S. Montgomery, Mary Nowlin, Anna Johnson, Stephanie Ferrante, James E. Montie, Ann Arbor, MI, William Johnston, Novi, MI, Mohammad Jafri, Bradley Rosenberg, Royal Oak, MI, Richard Sarle, Lansing, MI, Arvin K. George, for the Michigan Urological Surgery Improvement Collaborative, Ann Arbor, MI

Udit Singhal, MD
University of Michigan
Podium Presenter(s)
Introduction: The opioid epidemic has intensified focus on alternative pain management strategies after surgery. While prior findings have shown a decrease in opioid prescriptions after implementation of an opioid-limited pathway after radical prostatectomy (RP), minimal data exist evaluating a completely opioid-free pathway. We report on the statewide implementation of the Michigan opioid-free pain optimization pathway (MPOP) after RP, and determine the impact on post-operative opioid consumption and pain control.
Methods: MPOP was developed statewide in collaboration with the Michigan Opioid Prescribing Engagement Network and implemented starting October 2020. Baseline pain and opioid use were assessed preoperatively and 1-month post-RP. Opioid prescribing pre- and post-MPOP implementation was evaluated, including need for opioid prescription at discharge, refills, new outpatient opioid use, total opioid use, and overall pain control. Opioids were converted to total morphine milligram equivalents (MME) for standardization. Proportions were compared with the Chi-squared test and continuous measures with the Wilcoxon rank-sum test.
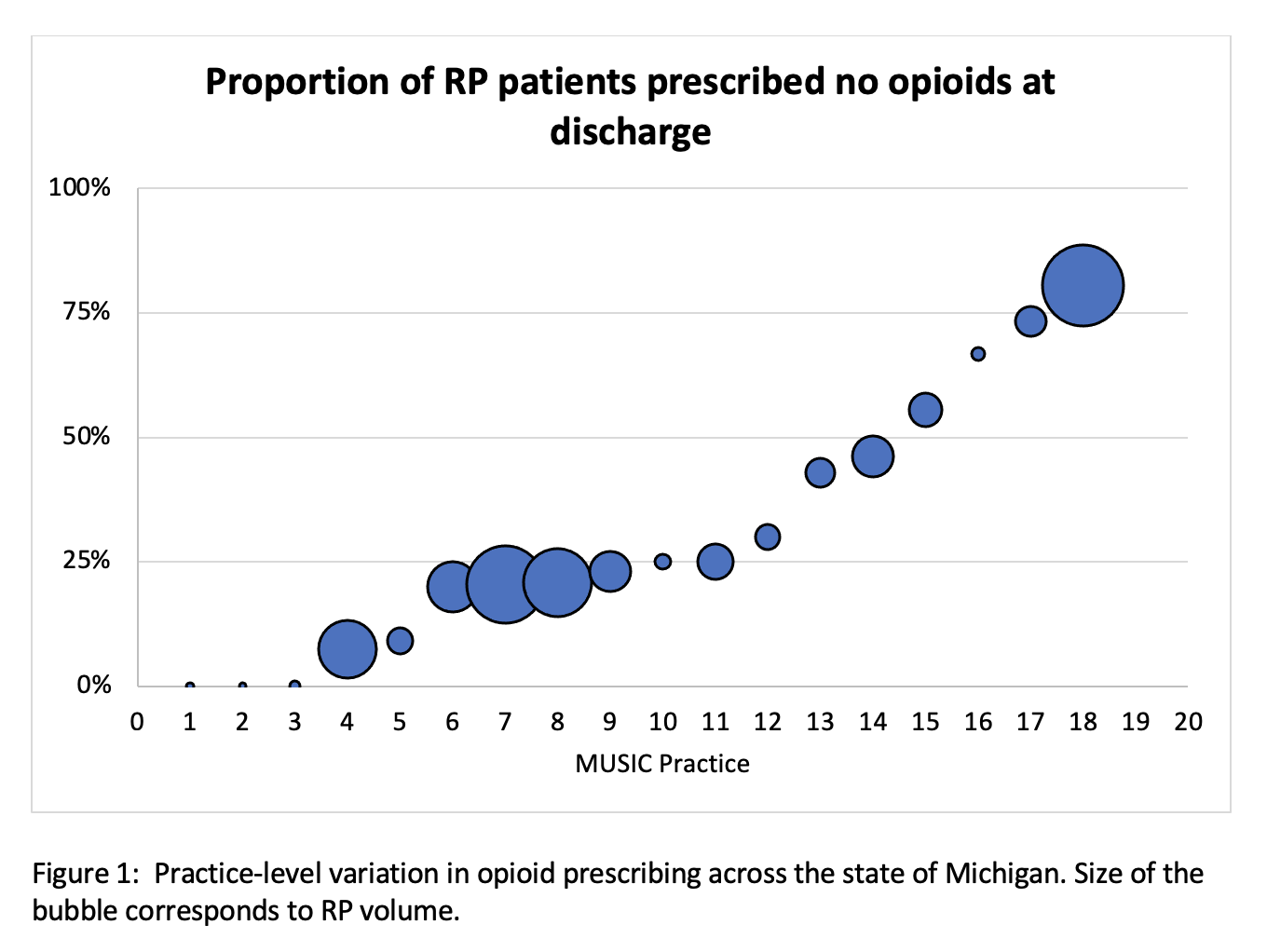
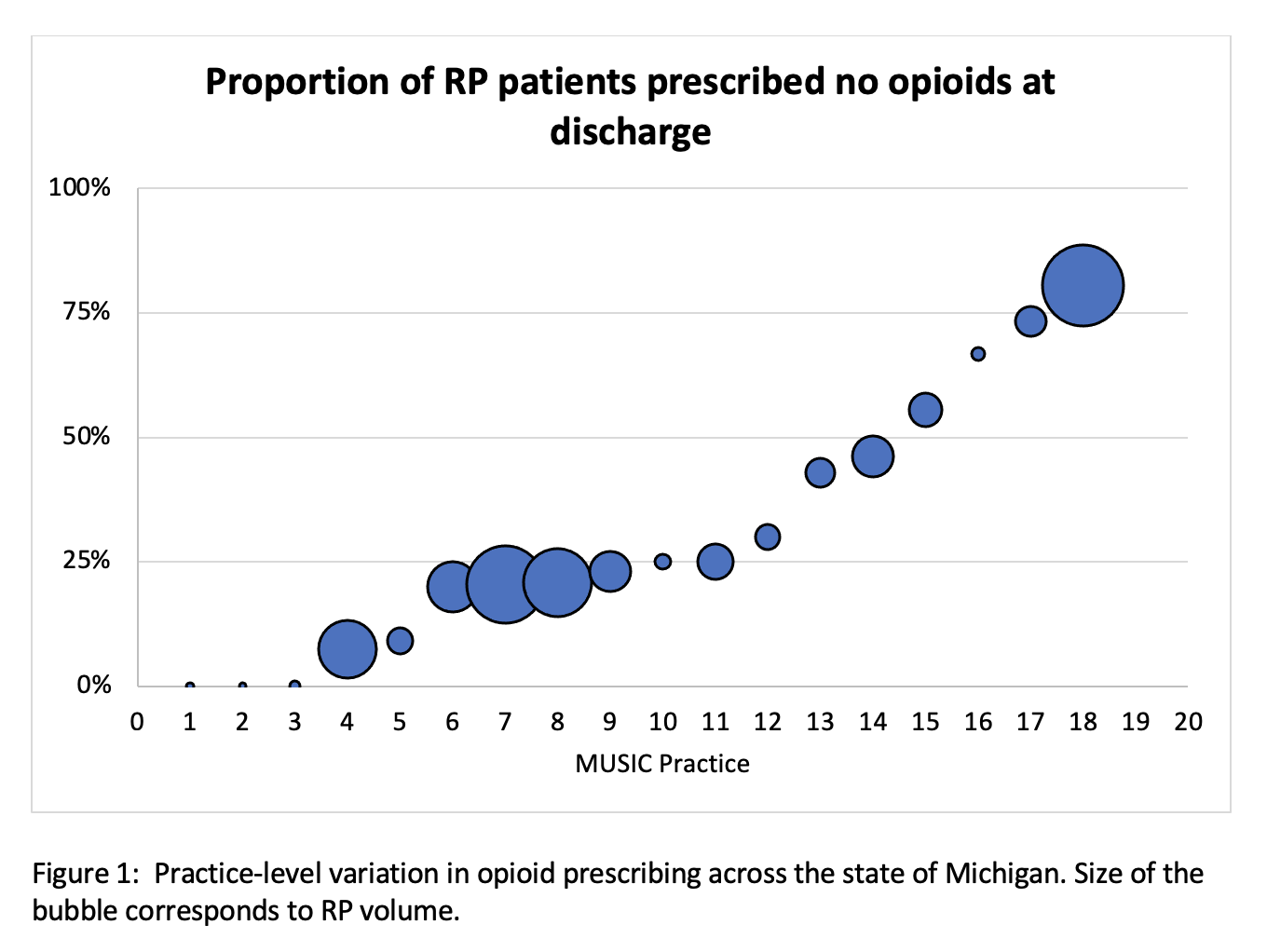
Results: A total of 2286 patients from 24 practices who underwent RP and completed the 1-month PRO survey were included. Proportion of patients by contributing practice discharged on the opioid-free pathway ranged from 0% to 81% (Figure 1). Prior to MPOP implementation, 82% (n=1460/1782) of patients were prescribed opioids at discharge, compared to 56% (281/504) post-MPOP (p < 0.001). After MPOP implementation, 2.7% of those discharged without opioids requested a prescription within 30 days. Among patients who received opioids, median opioid prescriptions remained stable pre vs post implementation (median=45 MME/patient, IQR 37.5-75). No significant differences were observed in postoperative pain scores between patients treated before vs after MPOP implementation (p=0.13). An estimated 16,000 fewer tablets of 5 mg oxycodone were prescribed due to MPOP implementation.
Conclusions: Implementation of a statewide opioid-free pain optimization pathway after RP led to decreased opioid prescriptions at discharge, reduced opioid consumption, and similar overall pain control reported by patients.
Source of Funding: Blue Cross Blue Shield of Michigan
Methods: MPOP was developed statewide in collaboration with the Michigan Opioid Prescribing Engagement Network and implemented starting October 2020. Baseline pain and opioid use were assessed preoperatively and 1-month post-RP. Opioid prescribing pre- and post-MPOP implementation was evaluated, including need for opioid prescription at discharge, refills, new outpatient opioid use, total opioid use, and overall pain control. Opioids were converted to total morphine milligram equivalents (MME) for standardization. Proportions were compared with the Chi-squared test and continuous measures with the Wilcoxon rank-sum test.
Results: A total of 2286 patients from 24 practices who underwent RP and completed the 1-month PRO survey were included. Proportion of patients by contributing practice discharged on the opioid-free pathway ranged from 0% to 81% (Figure 1). Prior to MPOP implementation, 82% (n=1460/1782) of patients were prescribed opioids at discharge, compared to 56% (281/504) post-MPOP (p < 0.001). After MPOP implementation, 2.7% of those discharged without opioids requested a prescription within 30 days. Among patients who received opioids, median opioid prescriptions remained stable pre vs post implementation (median=45 MME/patient, IQR 37.5-75). No significant differences were observed in postoperative pain scores between patients treated before vs after MPOP implementation (p=0.13). An estimated 16,000 fewer tablets of 5 mg oxycodone were prescribed due to MPOP implementation.
Conclusions: Implementation of a statewide opioid-free pain optimization pathway after RP led to decreased opioid prescriptions at discharge, reduced opioid consumption, and similar overall pain control reported by patients.
Source of Funding: Blue Cross Blue Shield of Michigan

.jpg)
.jpg)