Back
Poster, Podium & Video Sessions
Podium
PD55: Stone Disease: Surgical Therapy (including ESWL) IV
PD55-07: Outcomes and procedural costs following mini-percutaneous nephrolithotomy or flexible ureteroscopic lithotripsy for kidney stones between 1-2cm: Data from a prospective, randomized clinical trial
Monday, May 16, 2022
10:30 AM – 10:40 AM
Location: Room 252
Rahul Dutta*, Prabhakar Mithal, Ilan Klein, Manish Patel, Jorge Gutierrez-Aceves, Winston Salem, NC
Rahul Dutta, MD
Wake Forest School of Medicine
Podium Presenter(s)
Introduction: Both percutaneous nephrolithotomy (PCNL) and flexible ureteroscopic lithotripsy (URS) are options in treating patients with kidney stones that are unlikely to pass spontaneously. We sought to compare outcomes and hospital costs for patients randomized to mini-percutaneous nephrolithotomy (mPCNL, tract size 16.5 French) and URS for nephrolithiasis.
Methods: Patients who were candidates for both mPCNL and URS with a kidney stone between 1-2 cm located in the kidney were consented, enrolled, and randomized to a treatment group. Post-operative stone burden was assessed with low-dose CT scan between day 1 and 30 post-operatively. Hospital costs for operating room time, anesthesia time, and equipment (including equipment repairs) for the procedure were obtained.
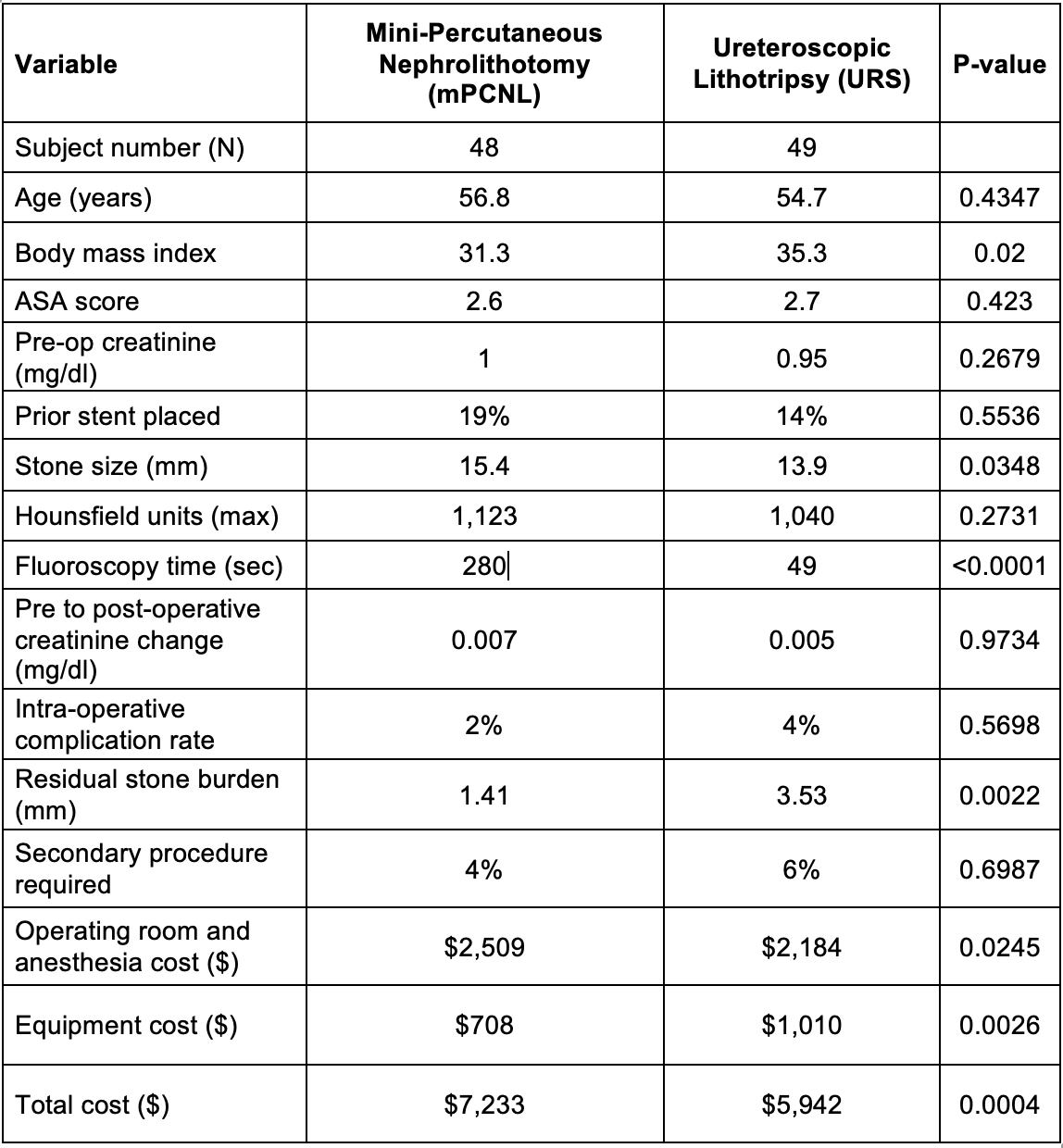
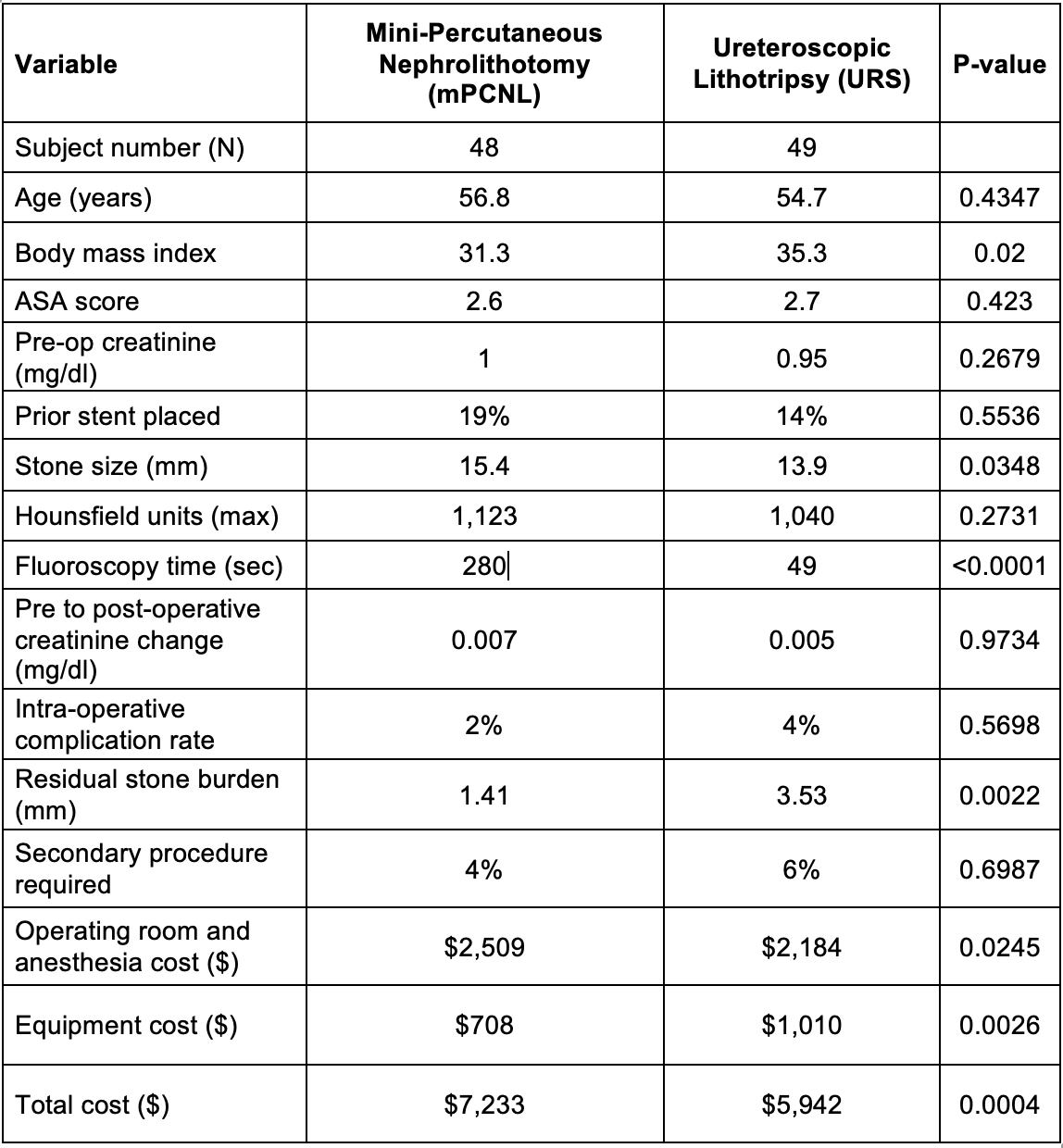
Results: A total of 97 patients were randomized to either mPCNL or URS. There were no significant differences between patient demographics, aside from a higher body mass index in the URS group (p=0.0200). The pre-operative stone burden was slightly higher in the mPCNL group (15.4 vs 13.9mm, p=0.0348). Fluoroscopy time was significantly higher in mPCNL procedures. There was no difference in intra-op complication rate or pre to post-operative creatinine change (p>0.05). Residual stone burden was lower in mPCNL group (1.4mm vs 3.5mm, p = 0022), though complications and necessity for secondary procedures did not vary (p>0.05). Operating room and anesthesia costs were higher for the mPCNL group, while equipment costs were higher for the URS group. Total direct and indirect costs were higher for the mPCNL group.
Conclusions: In this prospective randomized study, we found a lower residual stone burden in patients treated with mPCNL over URS for intrarenal stones 1-2cm in size. There were no differences in reoperations or complications. Total costs were higher for patients who underwent mPCNL.
Source of Funding: None
Methods: Patients who were candidates for both mPCNL and URS with a kidney stone between 1-2 cm located in the kidney were consented, enrolled, and randomized to a treatment group. Post-operative stone burden was assessed with low-dose CT scan between day 1 and 30 post-operatively. Hospital costs for operating room time, anesthesia time, and equipment (including equipment repairs) for the procedure were obtained.
Results: A total of 97 patients were randomized to either mPCNL or URS. There were no significant differences between patient demographics, aside from a higher body mass index in the URS group (p=0.0200). The pre-operative stone burden was slightly higher in the mPCNL group (15.4 vs 13.9mm, p=0.0348). Fluoroscopy time was significantly higher in mPCNL procedures. There was no difference in intra-op complication rate or pre to post-operative creatinine change (p>0.05). Residual stone burden was lower in mPCNL group (1.4mm vs 3.5mm, p = 0022), though complications and necessity for secondary procedures did not vary (p>0.05). Operating room and anesthesia costs were higher for the mPCNL group, while equipment costs were higher for the URS group. Total direct and indirect costs were higher for the mPCNL group.
Conclusions: In this prospective randomized study, we found a lower residual stone burden in patients treated with mPCNL over URS for intrarenal stones 1-2cm in size. There were no differences in reoperations or complications. Total costs were higher for patients who underwent mPCNL.
Source of Funding: None

.jpg)
.jpg)