Back
Poster, Podium & Video Sessions
Podium
PD55: Stone Disease: Surgical Therapy (including ESWL) IV
PD55-08: Optimization of Percutaneous Nephrolithotomy for a Free-Standing Ambulatory Surgery Center: Outcomes from 1200 Cases
Monday, May 16, 2022
10:40 AM – 10:50 AM
Location: Room 252
Daniel Rosen*, Meagan Dunne, Hanover, MD, Max Drescher, Baltimore, MD, Brian Panish, Liam Hatch, Washington, DC, Joel Abbott, Las Vegas, NV, Julio Davalos, Hanover, MD

Daniel C. Rosen, MD
Icahn School of Medicine at Mount Sinai
Podium Presenter(s)
Introduction: Percutaneous Nephrolithotomy (PCNL) is frequently used as the primary treatment modality for patients with large stones or challenging anatomy. It has evolved from an inpatient procedure to one that is now routinely performed in the outpatient setting. We aimed to identify the patients who were able to be treated in a free-standing ambulatory surgical center (ASC).
Methods: We analyzed patients who underwent PCNL or mini-PCNL from 2015-2021 by one of three surgeons. Patients were selected for ambulatory surgery if there was not a mandatory imperative for inpatient admission e.g. BMI>50 or severe cardiac or respiratory comorbidities. Patients were not excluded from the ASC based on stone burden or age. Generally, patients were administered an intercostal block and left with a double J stent at the end of the procedure and a foley catheter that was removed in the PACU. The tract was plugged with gelfoam/thrombin. Demographic, preoperative, and postoperative data was prospectively collected. Descriptive statistics were used for analysis.
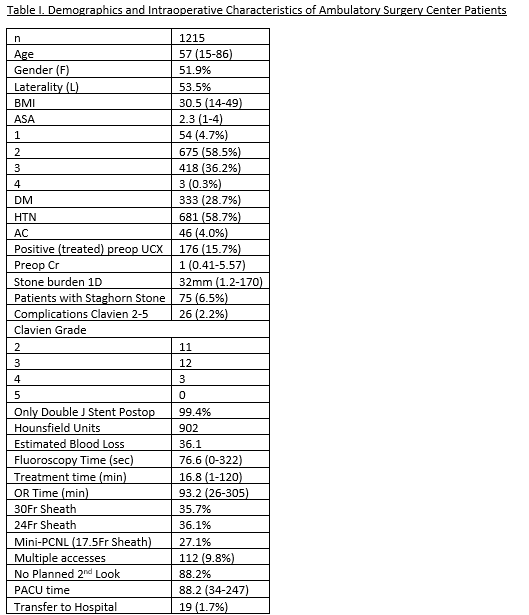
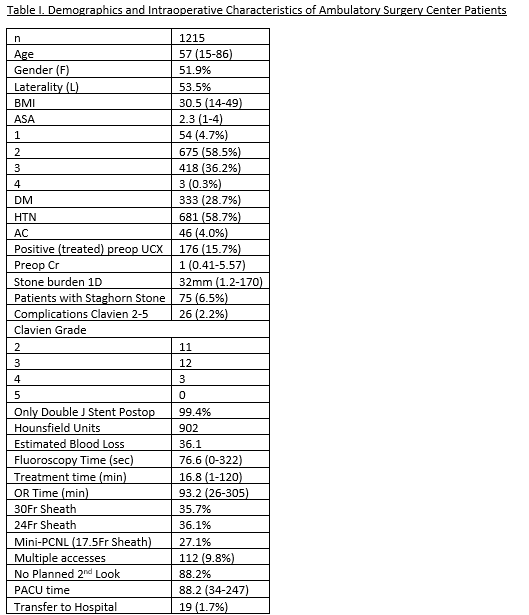
Results: 1215 patients were available for analysis. Demographic and intraoperative characteristics of the patients are shown in Table 1. Operative technique progressed over time with the usage of primarily smaller percutaneous access sheaths (24Fr replacing 30Fr as standard, and the implementation of common usage of 17.5Fr mini sheaths for smaller stones). Patients were generally limited to a maximum of 2 access sites. 1.7% of patients required transfer to the hospital postoperatively.
Conclusions: PCNL can safely and routinely be done as an outpatient procedure with low risk of hospital transfer. Patients should be carefully selected for inpatient procedure and admission based on comorbidities and prior anesthetic complication history.
Source of Funding: none
Methods: We analyzed patients who underwent PCNL or mini-PCNL from 2015-2021 by one of three surgeons. Patients were selected for ambulatory surgery if there was not a mandatory imperative for inpatient admission e.g. BMI>50 or severe cardiac or respiratory comorbidities. Patients were not excluded from the ASC based on stone burden or age. Generally, patients were administered an intercostal block and left with a double J stent at the end of the procedure and a foley catheter that was removed in the PACU. The tract was plugged with gelfoam/thrombin. Demographic, preoperative, and postoperative data was prospectively collected. Descriptive statistics were used for analysis.
Results: 1215 patients were available for analysis. Demographic and intraoperative characteristics of the patients are shown in Table 1. Operative technique progressed over time with the usage of primarily smaller percutaneous access sheaths (24Fr replacing 30Fr as standard, and the implementation of common usage of 17.5Fr mini sheaths for smaller stones). Patients were generally limited to a maximum of 2 access sites. 1.7% of patients required transfer to the hospital postoperatively.
Conclusions: PCNL can safely and routinely be done as an outpatient procedure with low risk of hospital transfer. Patients should be carefully selected for inpatient procedure and admission based on comorbidities and prior anesthetic complication history.
Source of Funding: none

.jpg)
.jpg)