Back
Poster, Podium & Video Sessions
Podium
PD56: Kidney Cancer: Localized: Surgical Therapy IV
PD56-03: Contemporary Perioperative Complications of Surgery for Renal Cell Carcinoma with Inferior Vena Cava Thrombectomy
Monday, May 16, 2022
9:50 AM – 10:00 AM
Location: Room 255
Daniel D. Joyce*, Andrew Zganjar, Vidit Sharma, Christine M. Lohse, R. Houston Thompson, Stephen A. Boorjian, John C. Cheville, Brian A. Costello, Bradley C. Leibovich, Rochester, MN

Daniel Joyce, MD
Mayo Clinic, Rochester, MN
Podium Presenter(s)
Introduction: Operative management of renal cell carcinoma (RCC) with venous tumor thrombus (VTT) extension into the inferior vena cava (level I-IV) continues to evolve in the setting of improved diagnostic imaging, technical surgical advancements, increased use of systemic therapies, and greater surgeon experience. Herein, therefore we provide a contemporary analysis of the Mayo Clinic experience with surgical management of RCC with VTT.
Methods: All adult patients who underwent open radical nephrectomy with thrombectomy for VTT level I-IV between 2000 and 2019 at Mayo Clinic, Rochester were included for analysis. Thirty-day complications and mortality were assessed, with major complications defined as those of Clavien grade III, IV, or V. Progression to chronic kidney disease (CKD) between left and right sided tumors was compared using a Cox proportional hazards regression model to identify potential intraoperative techniques associated with renal functional outcomes.
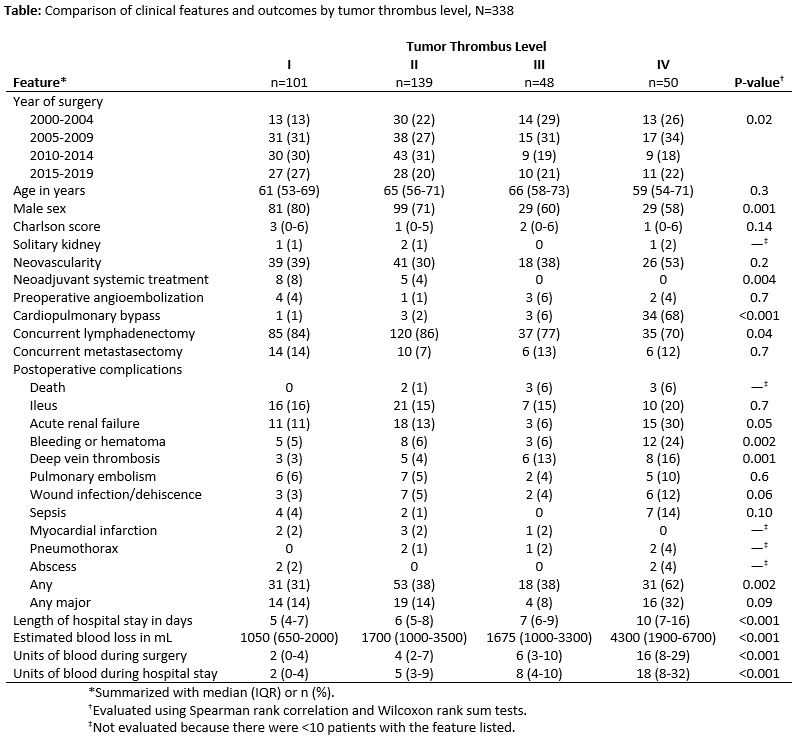
Results: Overall, 338 patients underwent radical nephrectomy with IVC thrombectomy. Of these 101 (30%), 139 (41%), 48 (14%), and 50 (15%) were VTT level I, II, III, and IV, respectively. Median age at surgery was 63 years (IQR 54-71) with the majority possessing an ECOG performance status of 0 or 1 (n=305, 90%) and few comorbidities (median CCI 2, IQR 0-6). Neoadjuvant systemic treatment was utilized in 13 (4%) patients, while preoperative embolization was performed in 10 (3%). The risk of major complications for level I, II, III, and IV VTT was 14% (n=14), 14% (n=19), 8% (n=4), and 32% (n=16) and perioperative death occurred in 0%, 1%, 6%, and 6%, respectively (Table). Complications remained highest for level IV thrombi after adjusting for age, sex, and comorbidity (odds ratio 3.02; 95% CI 1.50-6.07; p=0.002). While patients with right-sided tumors were more likely to develop CKD compared with those with left-sided tumors, this difference did not reach statistical significance (hazard ratio 1.21; 95% CI 0.89-1.65; p=0.2).
Conclusions: Operative management of RCC with level IV VTT remains associated with significantly greater complication risk compared to levels I-III. Contemporary peri-operative death was <10% for all VTT levels.
Source of Funding: None
Methods: All adult patients who underwent open radical nephrectomy with thrombectomy for VTT level I-IV between 2000 and 2019 at Mayo Clinic, Rochester were included for analysis. Thirty-day complications and mortality were assessed, with major complications defined as those of Clavien grade III, IV, or V. Progression to chronic kidney disease (CKD) between left and right sided tumors was compared using a Cox proportional hazards regression model to identify potential intraoperative techniques associated with renal functional outcomes.
Results: Overall, 338 patients underwent radical nephrectomy with IVC thrombectomy. Of these 101 (30%), 139 (41%), 48 (14%), and 50 (15%) were VTT level I, II, III, and IV, respectively. Median age at surgery was 63 years (IQR 54-71) with the majority possessing an ECOG performance status of 0 or 1 (n=305, 90%) and few comorbidities (median CCI 2, IQR 0-6). Neoadjuvant systemic treatment was utilized in 13 (4%) patients, while preoperative embolization was performed in 10 (3%). The risk of major complications for level I, II, III, and IV VTT was 14% (n=14), 14% (n=19), 8% (n=4), and 32% (n=16) and perioperative death occurred in 0%, 1%, 6%, and 6%, respectively (Table). Complications remained highest for level IV thrombi after adjusting for age, sex, and comorbidity (odds ratio 3.02; 95% CI 1.50-6.07; p=0.002). While patients with right-sided tumors were more likely to develop CKD compared with those with left-sided tumors, this difference did not reach statistical significance (hazard ratio 1.21; 95% CI 0.89-1.65; p=0.2).
Conclusions: Operative management of RCC with level IV VTT remains associated with significantly greater complication risk compared to levels I-III. Contemporary peri-operative death was <10% for all VTT levels.
Source of Funding: None

.jpg)
.jpg)