Back
Poster, Podium & Video Sessions
Podium
PD56: Kidney Cancer: Localized: Surgical Therapy IV
PD56-05: Short and intermediate term inferior vena cava patency outcomes in patients undergoing radical nephrectomy and venous tumor thrombectomy for renal cell carcinoma
Monday, May 16, 2022
10:10 AM – 10:20 AM
Location: Room 255
Harshit Garg*, FURKAN DURSUN, ROBERT COOPER, HANZANG WANG, MICHAEL LISS, Ahmed Mansour, Ahmed Mansour, ROBERT SVATEK, RONALD RODRIGUEZ, DHARAM KAUSHIK, DEEPAK PRUTHI, San Antonio, TX
Harshit Garg, MD
FELLOW
University of Texas Health, San Antonio
Podium Presenter(s)
Introduction: The reconstruction of inferior vena cava (IVC) during Radical nephrectomy (RN) with venous tumor thrombectomy (VTT) is mostly done using primary closure or with a patch/graft. However, literature on patency after IVC reconstruction during RN is limited. We sought to evaluate the outcomes of IVC patency over short to intermediate term follow-up
Methods: A retrospective review of all patients undergoing RN with VTT from January 2013 to August 2018 was conducted. Patients were followed until death, last available follow-up or September 2021.The patency outcomes were studied using follow-up cross-sectional imaging. All patients were placed on aspirin 81mg for up to 1 year. Chi-Square test, Student’s t-test, and Kaplan Meier survival analysis was employed.
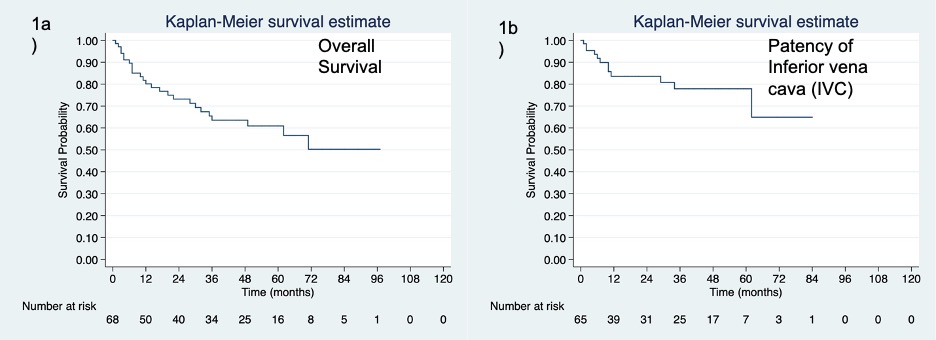
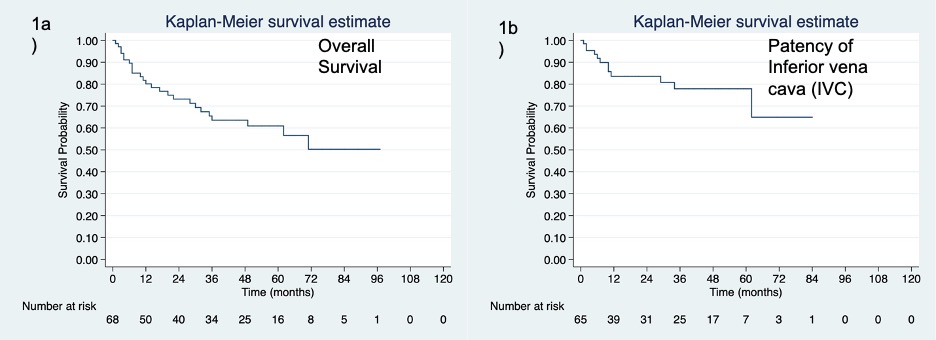
Results: Seventy-seven patients undergoing RN with VTT were included. Of these, one patient underwent stapling off IVC and was excluded. Of 76 patients, the mean (SD) age was 59.3(12.2) years. The mean Charlson comorbidity index was 6.2(2.5). Majority of the patients had right sided tumor (59.2%) and 46.2% had Mayo Classification Level III thrombus or higher. Twenty (26.3%) required veno-venous/cardiopulmonary bypass and 85.5% had clear cell RCC. The 30-day postoperative mortality rate was 3.9%. In terms of IVC reconstruction, 62 patients (81.5%) had IVC reconstruction, of which 59 patients (95.2%) underwent primary closure. At a median(IQR) follow-up of 20 (6-49) months, 21.5% patients developed caval occlusion. The 5-year IVC patency rate (IQR) was 77% (62%-87%). Supradiaphragmatic thrombectomies were associated with 44.4% caval occlusion rate as compared to 13.3% in infra-diaphragmatic thrombectomies (p=0.021). Among those with no patency, 5(8.1%) had recurrent tumor, 4 (6.4%) had recurrent thrombosis, and 2 (3.2%) developed fibrosis. The median 5-year overall survival (IQR) was 36% (23-50%). [Figure 1a] The median time (IQR) for caval occlusion was 8.5(3.5-20) months. [Figure 1b] No variable predicted caval patency. Patients who developed caval occlusion had significantly worse survival (HR=3.59, p=0.004) as compared to those without caval occlusion.
Conclusions: Primary caval repair results in high patency rates however among those who occlude survival is diminished.
Source of Funding: None
Methods: A retrospective review of all patients undergoing RN with VTT from January 2013 to August 2018 was conducted. Patients were followed until death, last available follow-up or September 2021.The patency outcomes were studied using follow-up cross-sectional imaging. All patients were placed on aspirin 81mg for up to 1 year. Chi-Square test, Student’s t-test, and Kaplan Meier survival analysis was employed.
Results: Seventy-seven patients undergoing RN with VTT were included. Of these, one patient underwent stapling off IVC and was excluded. Of 76 patients, the mean (SD) age was 59.3(12.2) years. The mean Charlson comorbidity index was 6.2(2.5). Majority of the patients had right sided tumor (59.2%) and 46.2% had Mayo Classification Level III thrombus or higher. Twenty (26.3%) required veno-venous/cardiopulmonary bypass and 85.5% had clear cell RCC. The 30-day postoperative mortality rate was 3.9%. In terms of IVC reconstruction, 62 patients (81.5%) had IVC reconstruction, of which 59 patients (95.2%) underwent primary closure. At a median(IQR) follow-up of 20 (6-49) months, 21.5% patients developed caval occlusion. The 5-year IVC patency rate (IQR) was 77% (62%-87%). Supradiaphragmatic thrombectomies were associated with 44.4% caval occlusion rate as compared to 13.3% in infra-diaphragmatic thrombectomies (p=0.021). Among those with no patency, 5(8.1%) had recurrent tumor, 4 (6.4%) had recurrent thrombosis, and 2 (3.2%) developed fibrosis. The median 5-year overall survival (IQR) was 36% (23-50%). [Figure 1a] The median time (IQR) for caval occlusion was 8.5(3.5-20) months. [Figure 1b] No variable predicted caval patency. Patients who developed caval occlusion had significantly worse survival (HR=3.59, p=0.004) as compared to those without caval occlusion.
Conclusions: Primary caval repair results in high patency rates however among those who occlude survival is diminished.
Source of Funding: None

.jpg)
.jpg)