Back
Poster, Podium & Video Sessions
Podium
PD57: Prostate Cancer: Detection & Screening VI
PD57-01: Multi-Institutional Analysis of Clinical and Imaging Risk Factors for Detecting Clinically Significant Prostate Cancer in Men with PI-RADS 3 Lesions
Monday, May 16, 2022
9:30 AM – 9:40 AM
Location: Room 245
Andrew Fang*, Luke Shumaker, Kimberly Martin, Birmingham, AL, Okechukwu Onah, Jamaal Jackson, Chicago, IL, Ghazal Khajir, New Haven, CT, Richard Fan, Stanford, CA, Nachiketh Soodana-Prakash, Miami, FL, Hiten Patel, Srinivas Vourganti, Chicago, IL, Christopher Filson, Atlanta, GA, Preston Sprenkle, New Haven, CT, Geoffrey Sonn, Stanford, CA, Sanoj Punnen, Miami, FL, Gopal Gupta, Chicago, IL, Soroush Rais-Bahrami, Birmingham, AL
.jpg)
Andrew Fang, MD
University of Alabama at Birmingham
Podium Presenter(s)
Introduction: While, it is standard to biopsy Prostate Imaging Reporting and Data System (PIRADS) 3 lesions, most do not contain clinically significant prostate cancer (CSPCa, Grade Group =2). We aim to identify clinical and magnetic resonance imaging (MRI) risk factors that predict CSPCa in men with PIRADS 3 lesions.
Methods: In this multi-institutional study, we reviewed men who underwent MRI targeted biopsy for a PIRADS 3 lesion with the primary endpoint being the detection of CSPCa. Multivariable logistic regression models with goodness of fit testing were used to identify variables associated with CSPCa. The probability of detecting CSPCa was plotted on a heatmap based on biopsy naïve (BN), previous negative biopsy (PNB), and active surveillance (AS) status. Receiver operating curves and decision curve analyses were calculated using separate training and validation cohorts.
Results: Of the 1,784 men reviewed, 1,537 were included in the training cohort and 247 in the validation cohort. The 309 (17.3%) men with CSPCa had higher PSA (9.2±8.5 versus 7.4±5.6 ng/ml, p<0.01), lower MRI prostate volume (52.7±29.8 versus 66.4±37.2 ml, p<0.01), and higher PSA density (0.21±0.2 versus 0.13±0.11 ng/ml2, p<0.01) than men without CSPCa. Multivariable analysis revealed PSA density (OR=32.4, 95%CI:13.1-84.0, p<0.01), age (OR=1.05, 95%CI:1.02-1.07, p<0.01), BN (OR=2.9; 95%CI:2.1-4.2, p<0.01), and AS (OR=1.6, 95%CI:1.1-2.0, p<0.01) were independently associated with CSPCa, while a PNB was negatively associated (OR=0.4, 95%CI:0.3-0.5, p<0.01). Application of the model to the validation cohort resulted in an area under the curve of 0.74. Using a predicted risk threshold of 12.5%, 26% of biopsies could have been avoided while detecting 95% of CSPCa.
Conclusions: Of men with PIRADS 3 lesions, elevated PSA density, older age, BN, and AS are more likely to be diagnosed with CSPCa. PNB was less likely to have CSPCa. Utilization of a PIRADS 3 model can avoid biopsies while missing few cases of CSPCa.
Source of Funding: n/a
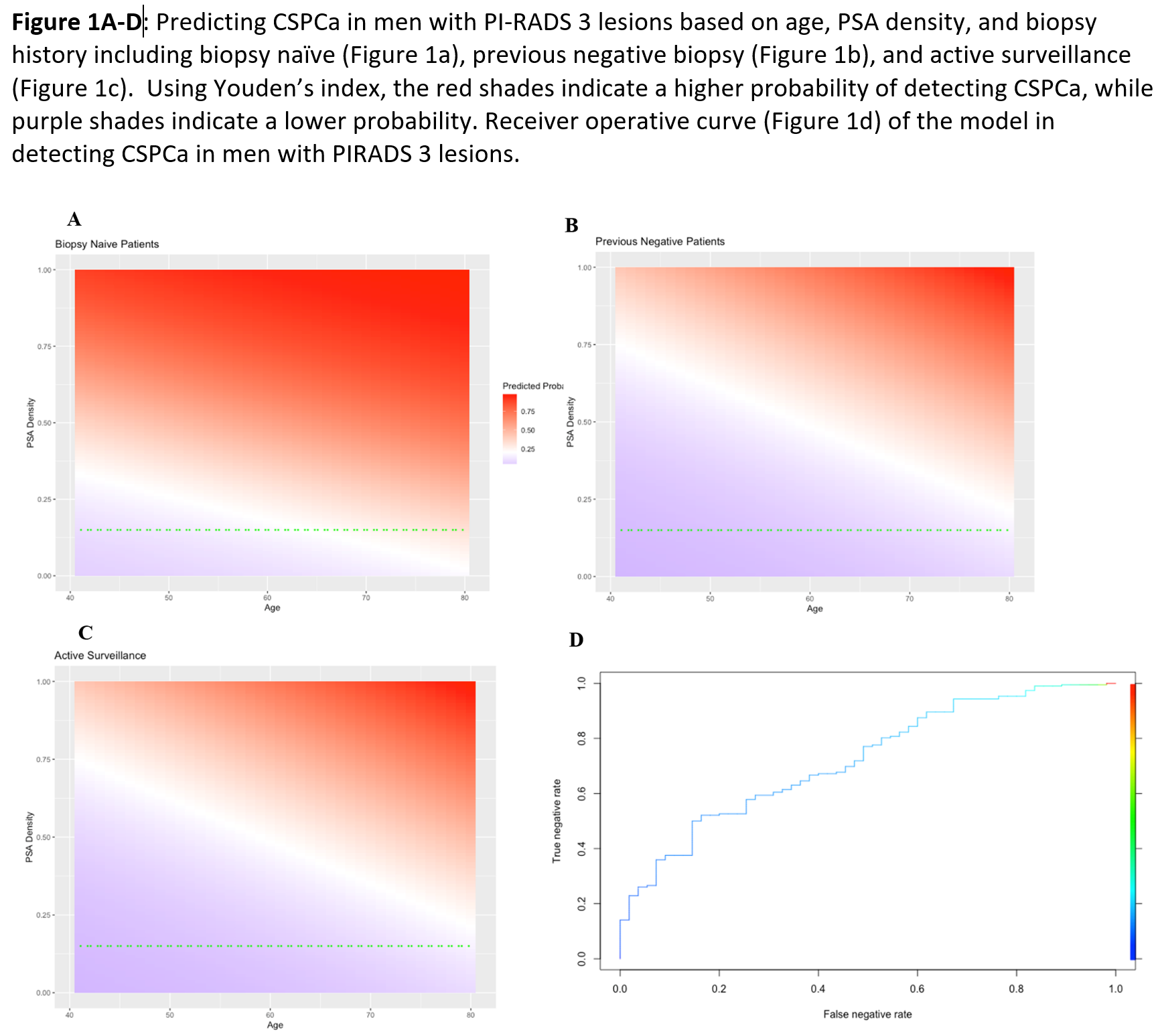
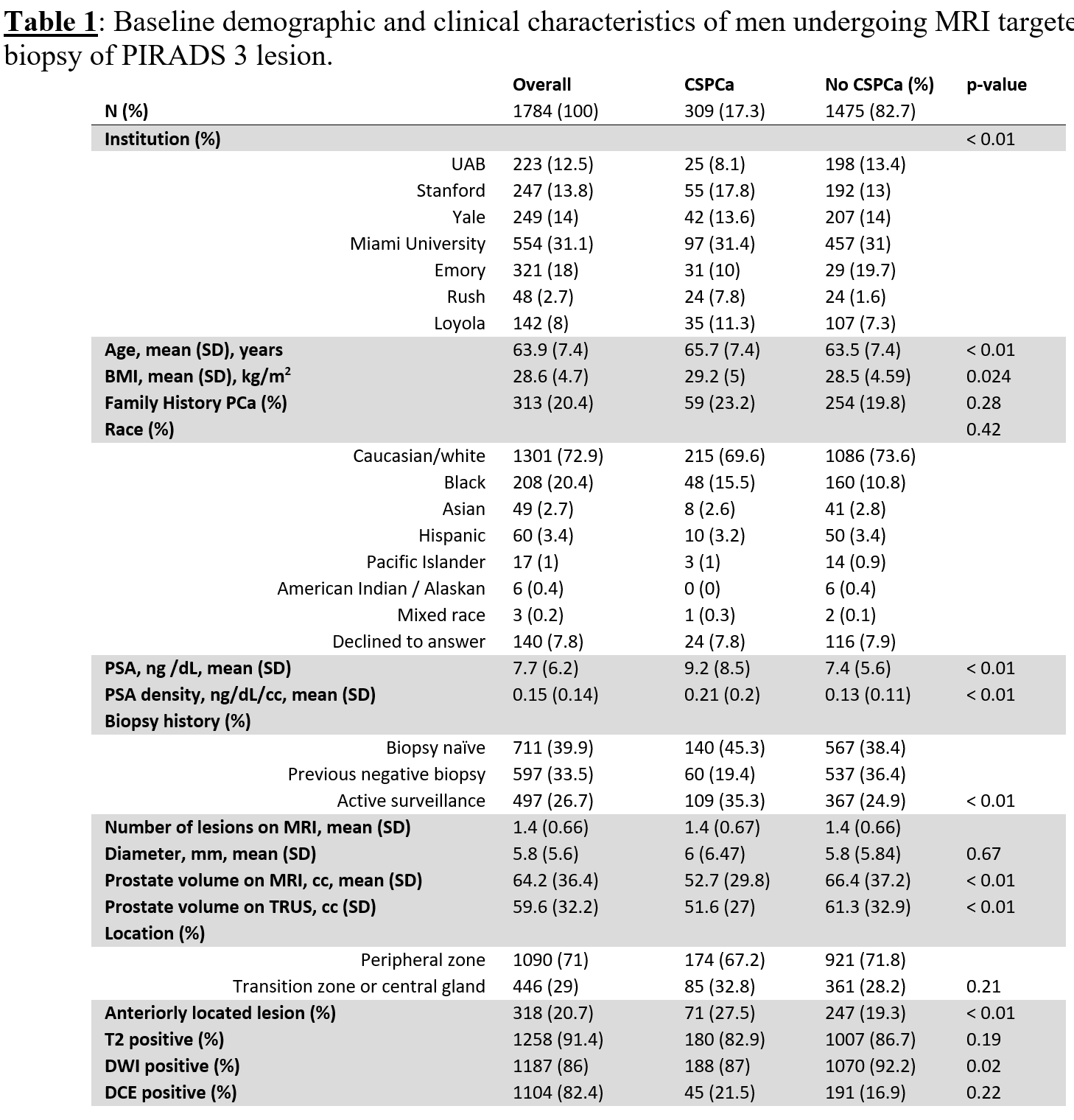
Methods: In this multi-institutional study, we reviewed men who underwent MRI targeted biopsy for a PIRADS 3 lesion with the primary endpoint being the detection of CSPCa. Multivariable logistic regression models with goodness of fit testing were used to identify variables associated with CSPCa. The probability of detecting CSPCa was plotted on a heatmap based on biopsy naïve (BN), previous negative biopsy (PNB), and active surveillance (AS) status. Receiver operating curves and decision curve analyses were calculated using separate training and validation cohorts.
Results: Of the 1,784 men reviewed, 1,537 were included in the training cohort and 247 in the validation cohort. The 309 (17.3%) men with CSPCa had higher PSA (9.2±8.5 versus 7.4±5.6 ng/ml, p<0.01), lower MRI prostate volume (52.7±29.8 versus 66.4±37.2 ml, p<0.01), and higher PSA density (0.21±0.2 versus 0.13±0.11 ng/ml2, p<0.01) than men without CSPCa. Multivariable analysis revealed PSA density (OR=32.4, 95%CI:13.1-84.0, p<0.01), age (OR=1.05, 95%CI:1.02-1.07, p<0.01), BN (OR=2.9; 95%CI:2.1-4.2, p<0.01), and AS (OR=1.6, 95%CI:1.1-2.0, p<0.01) were independently associated with CSPCa, while a PNB was negatively associated (OR=0.4, 95%CI:0.3-0.5, p<0.01). Application of the model to the validation cohort resulted in an area under the curve of 0.74. Using a predicted risk threshold of 12.5%, 26% of biopsies could have been avoided while detecting 95% of CSPCa.
Conclusions: Of men with PIRADS 3 lesions, elevated PSA density, older age, BN, and AS are more likely to be diagnosed with CSPCa. PNB was less likely to have CSPCa. Utilization of a PIRADS 3 model can avoid biopsies while missing few cases of CSPCa.
Source of Funding: n/a

.jpg)
.jpg)