Back
Poster, Podium & Video Sessions
Podium
PD57: Prostate Cancer: Detection & Screening VI
PD57-04: MRI-based PI-RADS score predicts ISUP upgrading and adverse pathology at radical prostatectomy in men with biopsy ISUP 1 prostate cancer
Monday, May 16, 2022
10:00 AM – 10:10 AM
Location: Room 245
Snir Dekalo, Tel Aviv, Israel, Jeremy Cepek*, London , Canada, Mario Sofer, Sophie Barnes, Ofer Yossepowitch, Roy Mano, Tel Aviv, Israel
- JC
Podium Presenter(s)
Introduction: To evaluate whether PI-RADS version 2 category 4 or 5 lesions in patients with ISUP 1 cancer on prostate biopsy predict ISUP upgrading and/or adverse pathology at radical prostatectomy.
Methods: We reviewed 127 consecutive patients who underwent 3-Tesla mpMRI and had ISUP 1 on biopsy followed by radical prostatectomy. mpMRI lesions were categorized according to the PI-RADS version 2 system. The study endpoints included ISUP upgrading to a clinically significant cancer (ISUP=2) and/or adverse pathology on prostatectomy. Associations between baseline characteristics and endpoints were evaluated with logistic regression analyses.
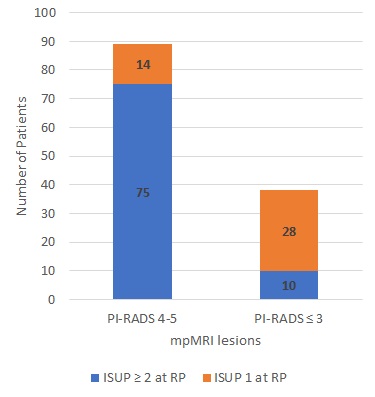
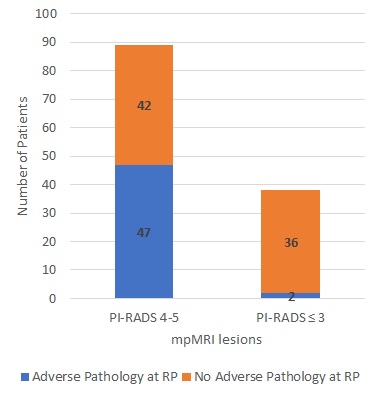
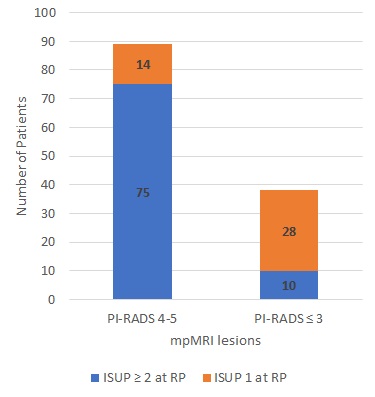
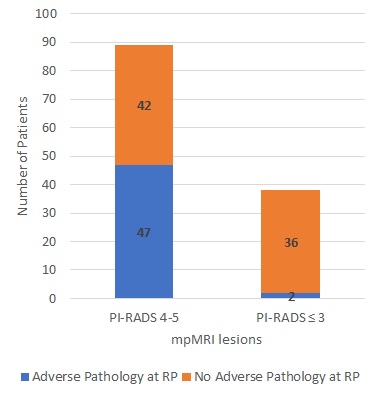
Results: PI-RADS 4 or 5 lesions were identified in 89 patients (70%). The rate of ISUP upgrading was higher among patients with PI-RADS 4-5 lesions (84%) compared to patients with equivocal or non-suspicious mpMRI findings (26%,p < 0.001). On multivariable logistic regression analysis both PI-RADS 4-5 lesions (OR 24.3, 95% CI 7.3, 80.5,p < 0.001) and stage T2 on DRE (OR 5.9, 95% CI 1.2, 29. 4,p=0.03) were independent predictors of upgrading. Men with PI-RADS 4-5 lesions had significantly higher rates of extra-prostatic extension (51% vs. 3%,p < 0.001) and positive surgical margins (16% vs. 3%.p=0.03). On multivariable logistic regression analysis PI-RADS 4-5 (OR 21.7, 95% CI 4.8, 99,p < 0.001) was the only independent predictor of adverse pathology.
Conclusions: Among patients with a biopsy ISUP 1 who underwent mpMRI, the presence of PI-RADS v2 4 or 5 lesions was a strong independent predictor of upgrading and adverse pathology. Future studies should evaluate whether incorporating mpMRI findings when selecting patients for active surveillance improves treatment outcome.
Source of Funding: None
Methods: We reviewed 127 consecutive patients who underwent 3-Tesla mpMRI and had ISUP 1 on biopsy followed by radical prostatectomy. mpMRI lesions were categorized according to the PI-RADS version 2 system. The study endpoints included ISUP upgrading to a clinically significant cancer (ISUP=2) and/or adverse pathology on prostatectomy. Associations between baseline characteristics and endpoints were evaluated with logistic regression analyses.
Results: PI-RADS 4 or 5 lesions were identified in 89 patients (70%). The rate of ISUP upgrading was higher among patients with PI-RADS 4-5 lesions (84%) compared to patients with equivocal or non-suspicious mpMRI findings (26%,p < 0.001). On multivariable logistic regression analysis both PI-RADS 4-5 lesions (OR 24.3, 95% CI 7.3, 80.5,p < 0.001) and stage T2 on DRE (OR 5.9, 95% CI 1.2, 29. 4,p=0.03) were independent predictors of upgrading. Men with PI-RADS 4-5 lesions had significantly higher rates of extra-prostatic extension (51% vs. 3%,p < 0.001) and positive surgical margins (16% vs. 3%.p=0.03). On multivariable logistic regression analysis PI-RADS 4-5 (OR 21.7, 95% CI 4.8, 99,p < 0.001) was the only independent predictor of adverse pathology.
Conclusions: Among patients with a biopsy ISUP 1 who underwent mpMRI, the presence of PI-RADS v2 4 or 5 lesions was a strong independent predictor of upgrading and adverse pathology. Future studies should evaluate whether incorporating mpMRI findings when selecting patients for active surveillance improves treatment outcome.
Source of Funding: None

.jpg)
.jpg)