Back
Poster, Podium & Video Sessions
Podium
PD57: Prostate Cancer: Detection & Screening VI
PD57-05: A Race-Stratified Analysis of the Accuracy of Prostate MRI in Biopsy Naive Men
Monday, May 16, 2022
10:10 AM – 10:20 AM
Location: Room 245
Julio Meza*, Rilwan Babajide, Ragheed Saoud, Josephine Abelleria, Irene Helenowski, Adam Murphy, Jeanne Horowitz, David Casalino, Chicago, IL
- JM
Podium Presenter(s)
Introduction: The Prostate Imaging Reporting and Data System (PIRADS) has shown promise in improving the detection of Gleason grade group (GG) 2-5 prostate cancer (PCa) and reducing the detection of indolent GG1 PCa. However, data on the performance of PIRADS in Black and Hispanic men is sparse. We evaluated the accuracy of PIRADS version 2.0 in detecting GG2-5 PCa in White, Black, and Hispanic men.
Methods: We performed a multicenter retrospective review of biopsy-naïve Black (n=108), White (n=108), and Hispanic (n=64) men who underwent prostate biopsy (PB) following multiparametric MRI. Sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) of PIRADS for GG2-5 PCa were calculated. Race-stratified binary logistic regression models for GG2-5 PCa using standard clinical variables and PIRADS were used to calculate area under the receiver operating characteristics curves (AUC).
Results: Rates of GG2-5 PCa were statistically similar between Blacks, Whites, and Hispanics (52.7% vs 42.6% vs 37.5% respectively, p = 0.12). Sensitivity and NPV were lower in Hispanic men compared to White men (87.5% vs 97.8%, p = 0.01; 70.0% vs 94.4%, p < 0.001). NPV was lower in Black men compared to White men (84.6 vs 94.4, p = 0.02). Specificity and PPV were similar in Black vs White men (21.6% vs 27.4%, p = 0.32; 57.9 vs 50.0%, p = 0.25) and White vs Hispanic men (27.4% vs 17.5%, p = 0.14; 50.0% vs 38.9%, p = 0.16).
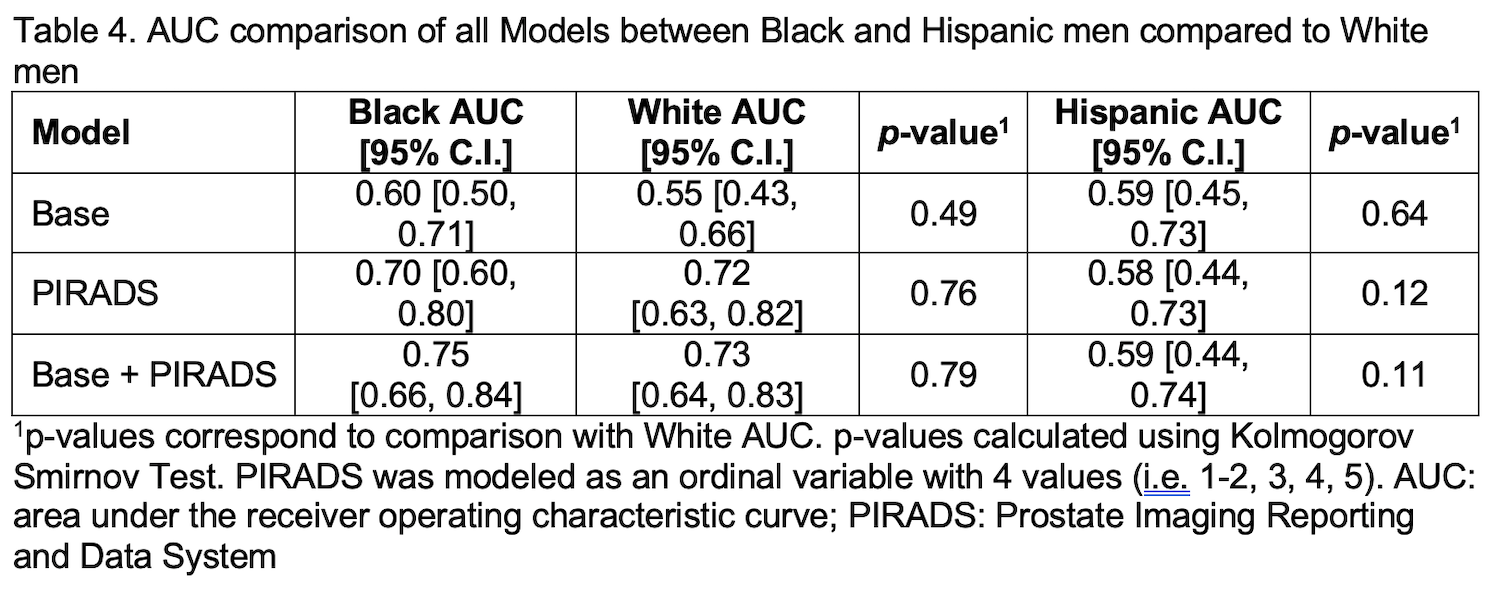
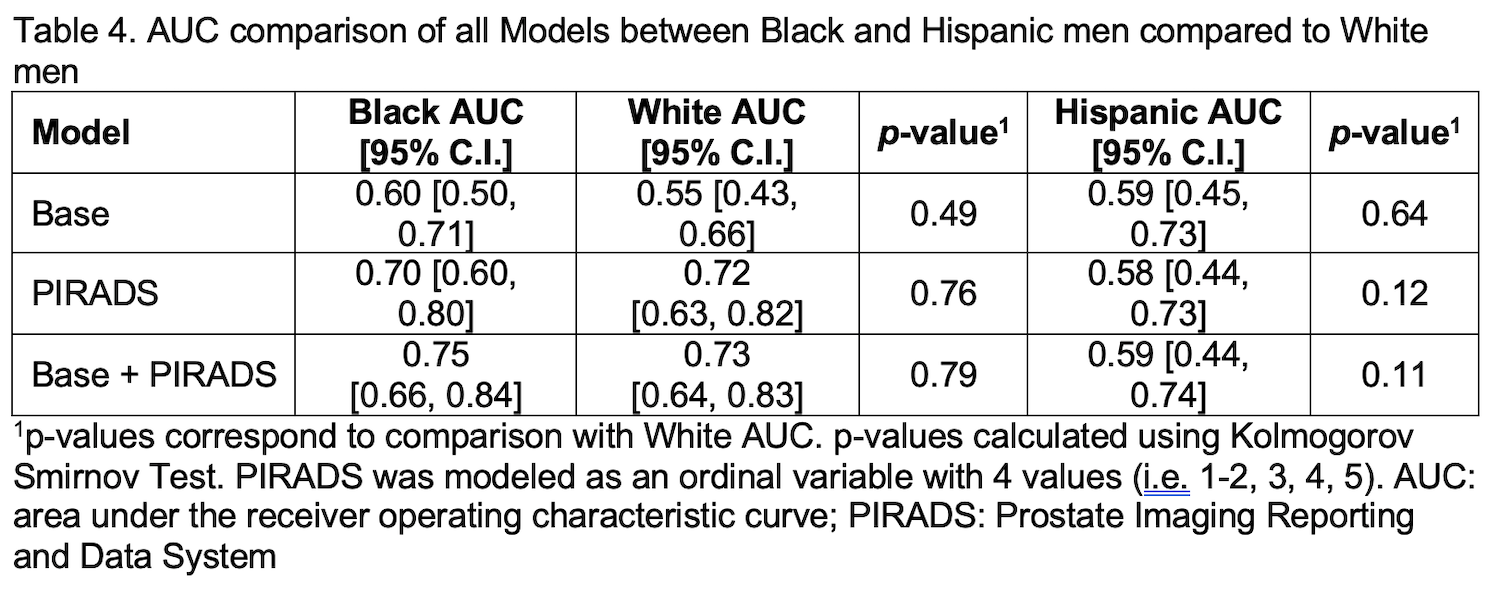
The AUCs of the PIRADS added to standard clinical data (age, PSA and suspicious prostate exam) were similar when comparing Black vs White men (0.75 vs 0.73, p = 0.79) and White vs Hispanic men (0.73 vs 0.59, p = 0.11). The AUCs for the Base model and PIRADS model alone were statistically similar when comparing Black vs White men and White vs Hispanic men.
Conclusions: The accuracy of the PIRADS and clinical data for detecting GG2-5 PCa seems statistically similar across race. However, there is concern that PIRADS 2.0 has lower NPV in Black and Hispanic men compared to White men. Prospective validation studies are needed.
Source of Funding: 1R01CA249973, National Cancer Institute

Methods: We performed a multicenter retrospective review of biopsy-naïve Black (n=108), White (n=108), and Hispanic (n=64) men who underwent prostate biopsy (PB) following multiparametric MRI. Sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) of PIRADS for GG2-5 PCa were calculated. Race-stratified binary logistic regression models for GG2-5 PCa using standard clinical variables and PIRADS were used to calculate area under the receiver operating characteristics curves (AUC).
Results: Rates of GG2-5 PCa were statistically similar between Blacks, Whites, and Hispanics (52.7% vs 42.6% vs 37.5% respectively, p = 0.12). Sensitivity and NPV were lower in Hispanic men compared to White men (87.5% vs 97.8%, p = 0.01; 70.0% vs 94.4%, p < 0.001). NPV was lower in Black men compared to White men (84.6 vs 94.4, p = 0.02). Specificity and PPV were similar in Black vs White men (21.6% vs 27.4%, p = 0.32; 57.9 vs 50.0%, p = 0.25) and White vs Hispanic men (27.4% vs 17.5%, p = 0.14; 50.0% vs 38.9%, p = 0.16).
The AUCs of the PIRADS added to standard clinical data (age, PSA and suspicious prostate exam) were similar when comparing Black vs White men (0.75 vs 0.73, p = 0.79) and White vs Hispanic men (0.73 vs 0.59, p = 0.11). The AUCs for the Base model and PIRADS model alone were statistically similar when comparing Black vs White men and White vs Hispanic men.
Conclusions: The accuracy of the PIRADS and clinical data for detecting GG2-5 PCa seems statistically similar across race. However, there is concern that PIRADS 2.0 has lower NPV in Black and Hispanic men compared to White men. Prospective validation studies are needed.
Source of Funding: 1R01CA249973, National Cancer Institute


.jpg)
.jpg)