Back
Poster, Podium & Video Sessions
Podium
PD58: Bladder Cancer: Upper Tract Transitional Cell Carcinoma II
PD58-07: Impact of Node Count on Survival Outcomes of Lymph Node Dissection in non-Metastatic Upper Tract Urothelial Carcinoma: Analysis of the ROBUUST Registry
Monday, May 16, 2022
2:00 PM – 2:10 PM
Location: Room 252
Kevin Hakimi*, La Jolla, CA, Umberto Carbonara, Richmond, VA, Hooman Djaladat, Los Angeles, CA, Reza Mehrazin, New York, NY, Daniel Eun, Adam Reese, Philadelphia, PA, Mark Gonzalgo, Miami, FL, Vitaly Margulis, Houston , TX, Robert Uzzo, Philadelphia, PA, James Porter, Seattle, WA, Chandru Sundaram, Indianapolis, IN, Firas Abdollah, Detroit, MI, Alexandre Mottrie, Aalast, Belgium, Riccardo Tellini, Florence , Italy, Matteo Ferro, Milan, Italy, Margaret Meagher, Ava Saidian, Arman Walia, La Jolla, CA, Alessandro Veccia, Richmond, VA, Alireza Ghoreifi, Giovanni Cacciamani, Los Angeles, CA, Amit Bhattu, Miami, FL, Xiaosong Meng, Houston , TX, Jason Farrow, Indianapolis, IN, Marcus Jamil, Detroit, MI, Andrea Minervini, Florence , Italy, Koon Rha, Seoul , Korea, Republic of, Zhenjie Wu, Shanghai , China, People's Republic of, Giuseppe Simone, Rome, Italy, Riccardo Autorino, Richmond, VA, Ithaar Derweesh, La Jolla, CA
- KH
Podium Presenter(s)
Introduction: Utility of lymph node dissection (LND) in localized upper tract urothelial carcinoma (UTUC) is controversial. We evaluated impact of lymph node count on survival outcomes in patients with non-metastatic UTUC using a multi-institutional database.
Methods: We retrospectively analyzed the ROBUUST (RObotic surgery for Upper Tract Urothelial Cancer Study) registry of patients undergoing robotic nephroureterectomy with clinical node negative disease (cN0). The cohort was divided into patients who did not undergo LND (pNx), patients who underwent LND with <10 negative LN removed (pN0 <10), and patients with =10 negative LN removed (pN0=10). Primary outcome was recurrence free survival (RFS). Secondary outcomes were overall survival (OS) and cancer-specific survival (CSS). Multivariable analyses (MVA) were conducted for predictors of survival outcomes and LN positivity. Kaplan-Meier analyses (KMA) were used to compare survival outcomes based on number of nodes removed.
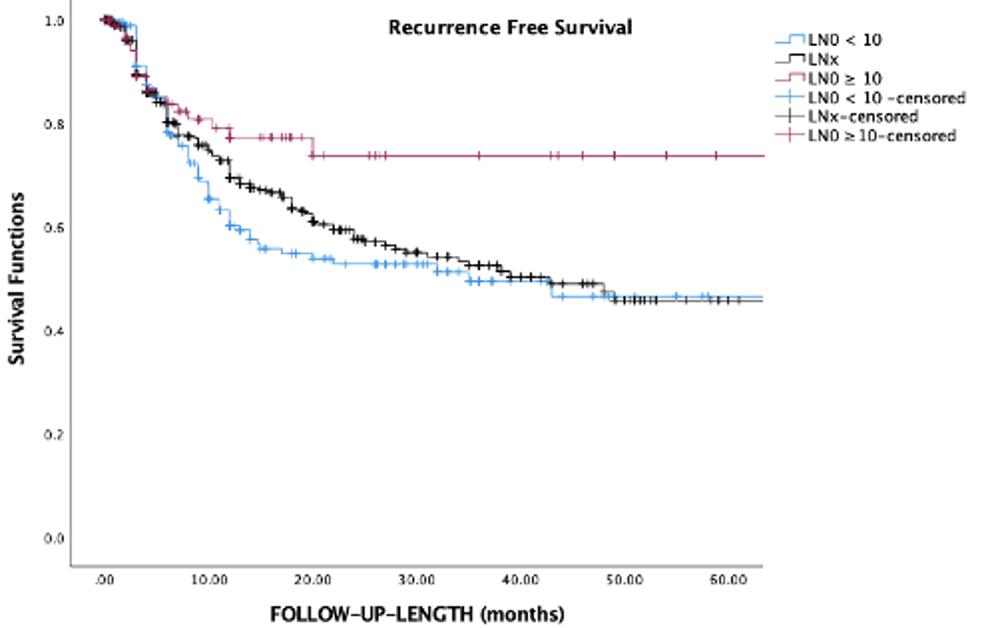
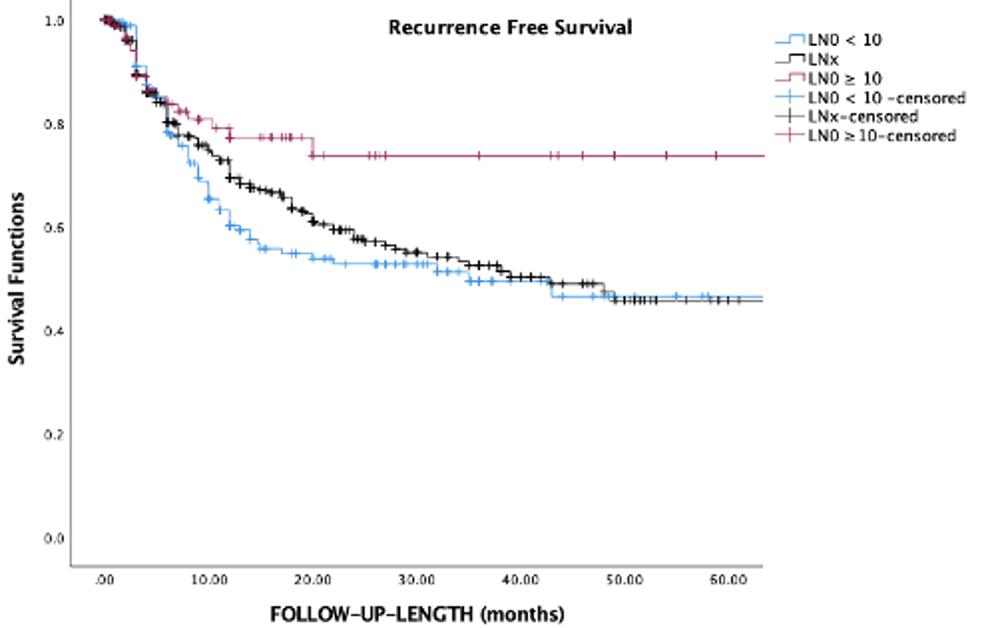
Results: 790 patients were analyzed [315 (39.9%) LND; median follow up 20 months]. Comparing pNx, pN0 <10, and pN0=10 patients, no significant differences were noted for high grade disease (p=0.091), tumor size (p=0.182), and multifocality (p=0.176); pN0=10 had lower incidence of recurrence (pNx 30.7%, pN0 <10 32.7%, pN0=10 18.9%; p=0.029). MVA noted pN0=10 (HR 0.77, p=0.029) was associated with decreased risk of recurrence, while multifocality (HR 1.62, p=0.003) was associated with increased risk. Nodal count was not independently associated with all-cause (p=0.704) and cancer-specific mortality (p=0.118). Predictors for LN positivity on MVA were high grade (OR 12.1, p=0.014) and tumor size >4.5cm (OR 2.12, p=0.005). KMA comparing survival outcomes of pNx, pN0 <10, and pN0=10 groups demonstrated improved 5-year RFS with pN0=10 (73% vs. pN0 <10 47% vs. pNx 39%; p=0.044; Figure). No differences were noted in 5-year OS (pN0=10 83% vs. pN0 <10 70% vs. pNx of 70%, p=0.854) and 5-year CSS (pN0=10 22%, pN0 <10 26% vs. pNx 22%, p=0.443).
Conclusions: Performance of LND with =10 nodes was associated with reduced risk of recurrence and improved RFS. Further investigation is requisite into impact of LN yield and for standardization of LND templates to optimize outcomes in non-metastatic UTUC.
Source of Funding: Stephen Weissman Kidney Cancer Fund
Methods: We retrospectively analyzed the ROBUUST (RObotic surgery for Upper Tract Urothelial Cancer Study) registry of patients undergoing robotic nephroureterectomy with clinical node negative disease (cN0). The cohort was divided into patients who did not undergo LND (pNx), patients who underwent LND with <10 negative LN removed (pN0 <10), and patients with =10 negative LN removed (pN0=10). Primary outcome was recurrence free survival (RFS). Secondary outcomes were overall survival (OS) and cancer-specific survival (CSS). Multivariable analyses (MVA) were conducted for predictors of survival outcomes and LN positivity. Kaplan-Meier analyses (KMA) were used to compare survival outcomes based on number of nodes removed.
Results: 790 patients were analyzed [315 (39.9%) LND; median follow up 20 months]. Comparing pNx, pN0 <10, and pN0=10 patients, no significant differences were noted for high grade disease (p=0.091), tumor size (p=0.182), and multifocality (p=0.176); pN0=10 had lower incidence of recurrence (pNx 30.7%, pN0 <10 32.7%, pN0=10 18.9%; p=0.029). MVA noted pN0=10 (HR 0.77, p=0.029) was associated with decreased risk of recurrence, while multifocality (HR 1.62, p=0.003) was associated with increased risk. Nodal count was not independently associated with all-cause (p=0.704) and cancer-specific mortality (p=0.118). Predictors for LN positivity on MVA were high grade (OR 12.1, p=0.014) and tumor size >4.5cm (OR 2.12, p=0.005). KMA comparing survival outcomes of pNx, pN0 <10, and pN0=10 groups demonstrated improved 5-year RFS with pN0=10 (73% vs. pN0 <10 47% vs. pNx 39%; p=0.044; Figure). No differences were noted in 5-year OS (pN0=10 83% vs. pN0 <10 70% vs. pNx of 70%, p=0.854) and 5-year CSS (pN0=10 22%, pN0 <10 26% vs. pNx 22%, p=0.443).
Conclusions: Performance of LND with =10 nodes was associated with reduced risk of recurrence and improved RFS. Further investigation is requisite into impact of LN yield and for standardization of LND templates to optimize outcomes in non-metastatic UTUC.
Source of Funding: Stephen Weissman Kidney Cancer Fund

.jpg)
.jpg)