Back
Poster, Podium & Video Sessions
Podium
PD58: Bladder Cancer: Upper Tract Transitional Cell Carcinoma II
PD58-11: Impact of Pre-operative Kidney Function on Survival Outcomes in Upper Tract Urothelial Carcinoma: Analysis of the ROBUUST Registry
Monday, May 16, 2022
2:40 PM – 2:50 PM
Location: Room 252
Kevin Hakimi*, La Jolla, CA, Umberto Carbonara, Richmond, VA, Hooman Djaladat, Los Angeles, CA, Reza Mehrazin, New York, NY, Daniel Eun, Adam Reese, Philadelphia, PA, Mark Gonzalgo, Miami, FL, Vitaly Margulis, Houston , TX, Robert Uzzo, Philadelphia, PA, James Porter, Seattle, WA, Chandru Sundaram, Indianapolis, IN, Firas Abdollah, Detroit, MI, Alexandre Mottrie, Aalast, Belgium, Riccardo Tellini, Florence , Italy, Matteo Ferro, Milan, Italy, Margaret Meagher, Ava Saidian, Arman Walia, La Jolla, CA, Alessandro Veccia, Richmond, VA, Alireza Ghoreifi, Giovanni Cacciamani, Los Angeles, CA, Amit Bhattu, Miami, FL, Xiaosong Meng, Houston , TX, Jason Farrow, Indianapolis, IN, Marcus Jamil, Detroit, MI, Andrea Minervini, Florence , Italy, Koon Rha, Seoul , Korea, Republic of, Zhenjie Wu, Shanghai , China, People's Republic of, Giuseppe Simone, Rome, Italy, Riccardo Autorino, Richmond, VA, Ithaar Derweesh, La Jolla, CA
- KH
Podium Presenter(s)
Introduction: Nephroureterectomy is cornerstone of management of localized and locally advanced upper tract urothelial carcinoma (UTUC), however impact of pre-operative renal functional status on outcomes is unknown. We evaluated the impact of pre-operative kidney function on outcomes in patients with UTUC using a multi-institutional database.
Methods: We retrospectively analyzed the ROBUUST (RObotic surgery for Upper Tract Urothelial Cancer Study) registry of UTUC patients undergoing nephroureterectomy from 2006-2019. The cohort was divided into patients with preoperative estimated glomerular filtration rate <60 mL/min/1.73m2 (eGFR <60) and preoperative eGFR =60 for descriptive and survival analyses. Primary outcome was overall survival (OS); secondary outcomes included cancer specific (CSS) and recurrence free survival (RFS). Cox regression multivariable analyses (MVA) were conducted for predictors of survival outcomes. Kaplan-Meier analyses (KMA) were utilized to compare survival outcomes between eGFR <60 and =60 groups.
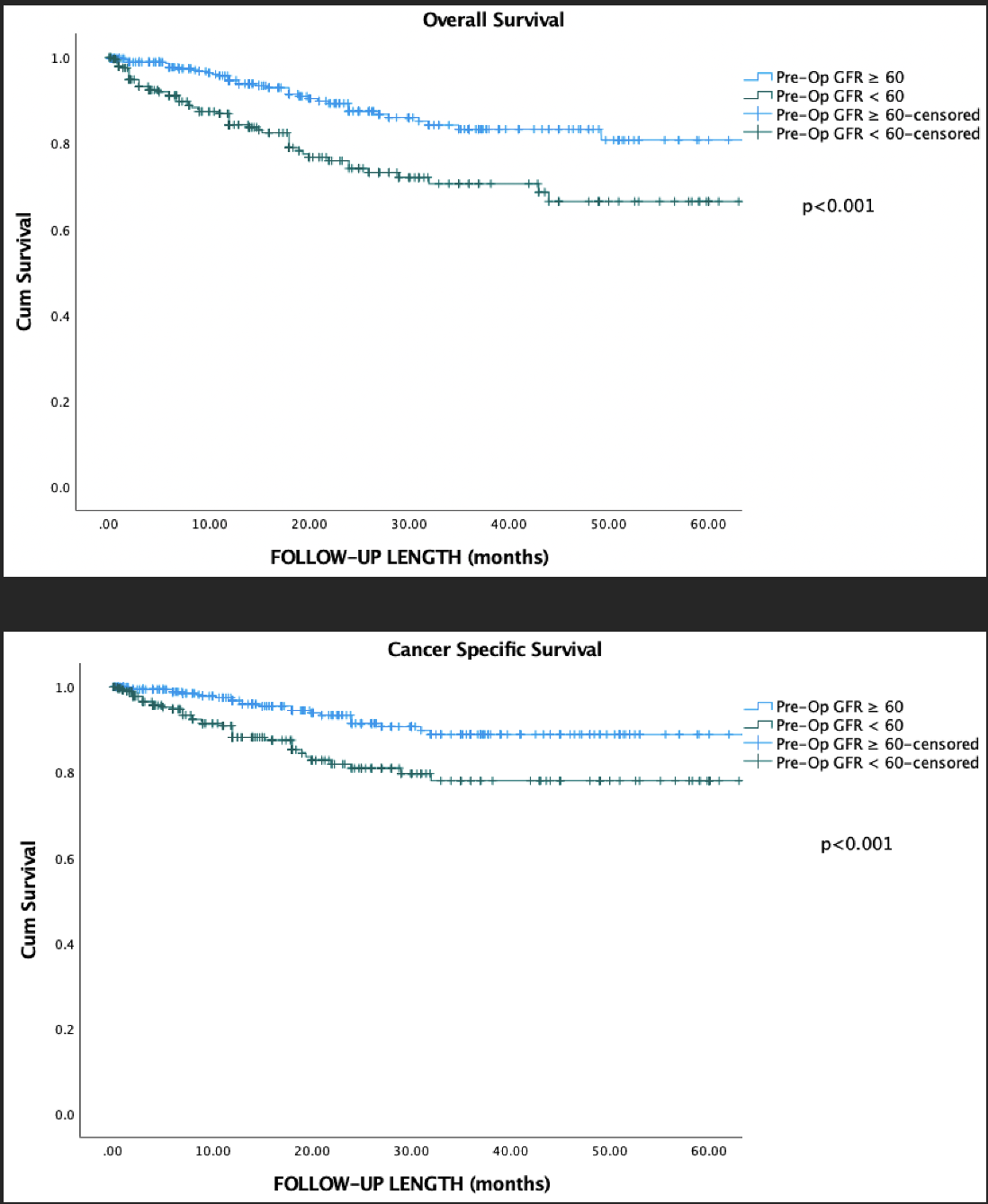
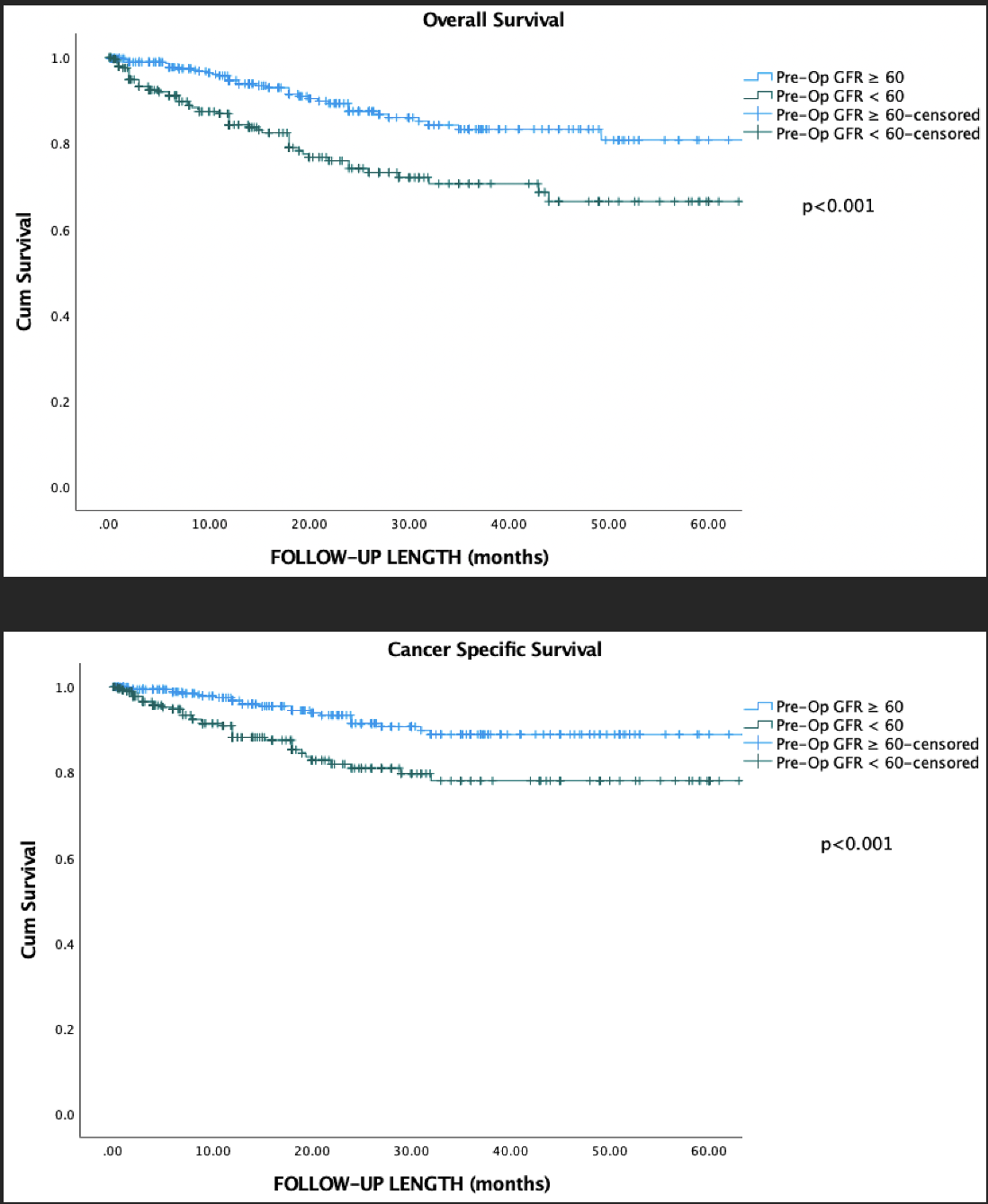
Results: We analyzed 767 patients (eGFR=60 400 patients/eGFR <60 309 patients; median follow up 19.1 months). Compared to eGFR =60, patients with eGFR <60 were older (p < 0.001) and had greater incidence of high tumor grade (86.9% vs. 80.9%, p=0.031) and lymphovascular invasion (24.8% vs. 17.3%, p=0.001). MVA identified pre-operative eGFR <60 (HR 2.1, p=0.017) and positive lymph nodes (HR 4.2, p<0.001) as risk factors for worsened all cause mortality, while pre-operative eGFR (HR 2.3, p=0.048) and positive lymph nodes (HR 7.0, p<0.001) are risk factors for worsened cancer specific mortality. MVA noted positive lymph nodes (HR 1.9, p=0.02) and systemic therapy (HR 1.6, p=0.018) as risk factors for recurrence. KMA comparing pre-op GFR=60 vs <60 demonstrated: 5-year OS of 81% and 68% (p < 0.001); 5-year CSS of 89% vs. 78% (p < 0.001) and 5-year RFS of 40% vs. 41% (p=0.107), respectively (Figure).
Conclusions: In this multi-institutional cohort of patients, worsened pre-operative functional status in patients with UTUC is associated with worsened oncologic survival outcomes post-nephroureterectomy. Our findings suggest consideration of preoperative renal function in risk stratification protocols to optimize outcomes in at risk patients.
Source of Funding: Stephen Weissman Kidney Cancer Fund
Methods: We retrospectively analyzed the ROBUUST (RObotic surgery for Upper Tract Urothelial Cancer Study) registry of UTUC patients undergoing nephroureterectomy from 2006-2019. The cohort was divided into patients with preoperative estimated glomerular filtration rate <60 mL/min/1.73m2 (eGFR <60) and preoperative eGFR =60 for descriptive and survival analyses. Primary outcome was overall survival (OS); secondary outcomes included cancer specific (CSS) and recurrence free survival (RFS). Cox regression multivariable analyses (MVA) were conducted for predictors of survival outcomes. Kaplan-Meier analyses (KMA) were utilized to compare survival outcomes between eGFR <60 and =60 groups.
Results: We analyzed 767 patients (eGFR=60 400 patients/eGFR <60 309 patients; median follow up 19.1 months). Compared to eGFR =60, patients with eGFR <60 were older (p < 0.001) and had greater incidence of high tumor grade (86.9% vs. 80.9%, p=0.031) and lymphovascular invasion (24.8% vs. 17.3%, p=0.001). MVA identified pre-operative eGFR <60 (HR 2.1, p=0.017) and positive lymph nodes (HR 4.2, p<0.001) as risk factors for worsened all cause mortality, while pre-operative eGFR (HR 2.3, p=0.048) and positive lymph nodes (HR 7.0, p<0.001) are risk factors for worsened cancer specific mortality. MVA noted positive lymph nodes (HR 1.9, p=0.02) and systemic therapy (HR 1.6, p=0.018) as risk factors for recurrence. KMA comparing pre-op GFR=60 vs <60 demonstrated: 5-year OS of 81% and 68% (p < 0.001); 5-year CSS of 89% vs. 78% (p < 0.001) and 5-year RFS of 40% vs. 41% (p=0.107), respectively (Figure).
Conclusions: In this multi-institutional cohort of patients, worsened pre-operative functional status in patients with UTUC is associated with worsened oncologic survival outcomes post-nephroureterectomy. Our findings suggest consideration of preoperative renal function in risk stratification protocols to optimize outcomes in at risk patients.
Source of Funding: Stephen Weissman Kidney Cancer Fund

.jpg)
.jpg)