Back
Poster, Podium & Video Sessions
Podium
PD59: Kidney Cancer: Advanced (including Drug Therapy) II
PD59-01: BAP1 Loss is Associated with Metastasis in Advanced Clear Cell Renal Cell Carcinoma
Monday, May 16, 2022
1:00 PM – 1:10 PM
Location: Room 255
Sari Khaleel*, Anne Reiner, Cameron Brennan, Ibrahim Hussain, Samuel Berman, Ari Hakimi, Nelson Moss, New York, NY
Sari S. Khaleel, MD, MSC
MSKCC
Podium Presenter(s)
Introduction: Mutations of the BAP1 tumor suppressor gene are found in 10-15% of clear cell renal cell carcinoma (ccRCC), portending a poor prognosis relative to BAP1-wildtype (BAP1-WT) tumors. However, it remains unclear if BAP1 loss predicts metastatic phenotype in ccRCC. We sought to assess the cumulative incidence of metastases in patients with BAP1-mutant (BAP1-MT) vs BAP1-WT ccRCC tumors.
Methods: We performed a retrospective review of 96 patients diagnosed with ccRCC with known BAP1 mutation status, managed at a tertiary care cancer center between 10/2001-9/2016, comparing patients with BAP1-MT (47 patients) to BAP1-WT (49 patients) tumors. For each patient, we retrieved clinical features and all metastatic events (MEs), accounting for the organ compartment and date of each individual ME noted on imaging and/or pathology reports. We hypothesized that BAP1-MT was associated with a higher likelihood of cumulative MEs overall, as well as a specific metastatic phenotype, defined as a predilection for cumulative MEs in one of two major compartments – bone or soft tissue (all non-bony compartments). Categorical and continuous outcomes were compared by BAP1 mutational status using Fisher’s exact test and Welch T-test, respectively, while cumulative incidence of MEs was compared between BAP1-MT and BAP1-WT using subdistribution hazard ratio (SD-HR) analysis. Analyses were performed using R package (R Foundation, v4.1).
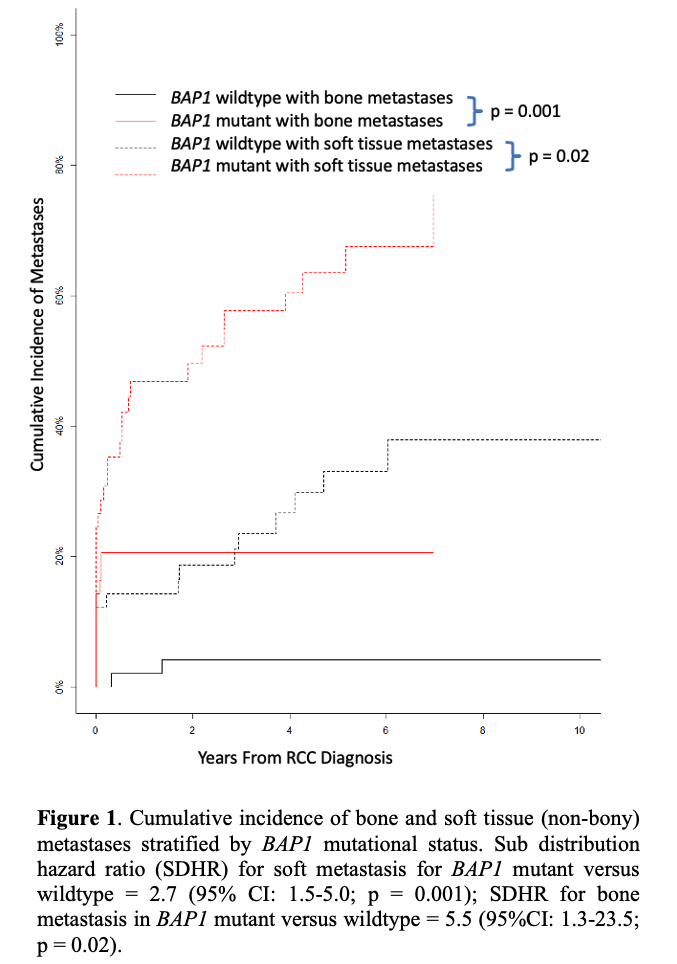
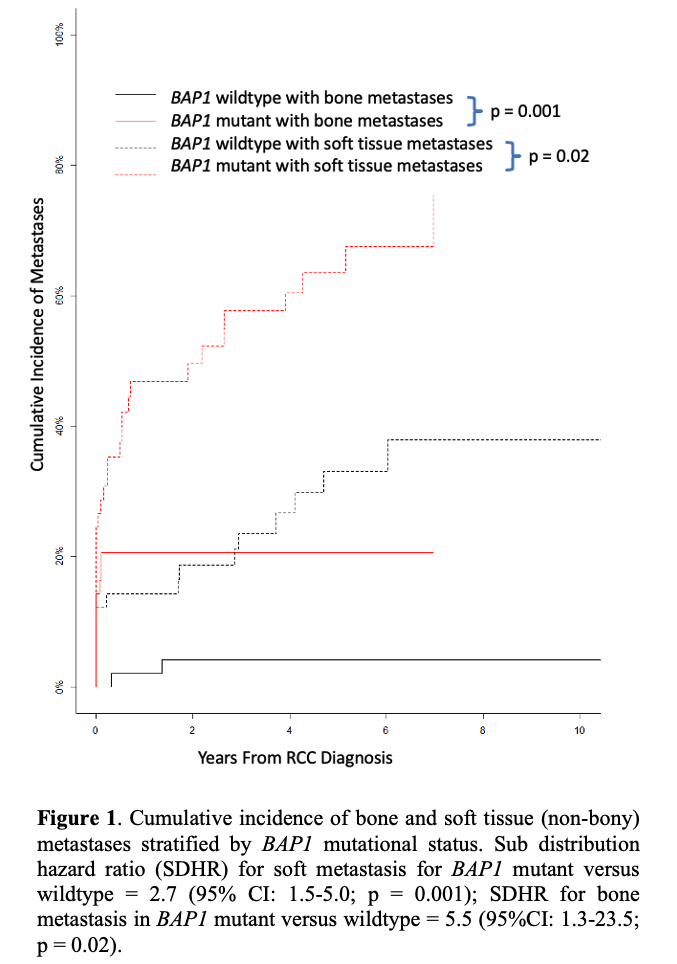
Results: Median patient age at diagnosis was 58 years, with 20 (20.8%) patients presenting with metastatic disease at the time of diagnosis. Most patients were males (62, 64.6%), and underwent nephrectomy (84, 87.5%). Median follow-up was 52 months [IQR 22.25 – 78.25 months]. BAP1-MT and BAP1-WT did not differ significantly by age or BMI (p > 0.05). BAP1-MT patients had a higher AJCC stage on nephrectomy (p < 0.0001), with higher overall cumulative MEs (SD-HR 2.1, 95% CI 1.0-4.5, p = 0.05). Specifically, we noted a high incidence of MEs in bone (SD-HR 5.5, p = 0.02, 95% CI 1.3-23.5) followed by soft tissue (SD-HR 2.7, p = 0.001, 95% CI 1.5 – 5.0) (Figure 1).
Conclusions: Mutations of the BAP1 gene were associated with higher stage disease and incidence of metastases overall, with a higher cumulative incidence of metastases in bone compared to soft tissue compartments, suggesting a potential metastatic phenotype for this mutation.
Source of Funding: None
Methods: We performed a retrospective review of 96 patients diagnosed with ccRCC with known BAP1 mutation status, managed at a tertiary care cancer center between 10/2001-9/2016, comparing patients with BAP1-MT (47 patients) to BAP1-WT (49 patients) tumors. For each patient, we retrieved clinical features and all metastatic events (MEs), accounting for the organ compartment and date of each individual ME noted on imaging and/or pathology reports. We hypothesized that BAP1-MT was associated with a higher likelihood of cumulative MEs overall, as well as a specific metastatic phenotype, defined as a predilection for cumulative MEs in one of two major compartments – bone or soft tissue (all non-bony compartments). Categorical and continuous outcomes were compared by BAP1 mutational status using Fisher’s exact test and Welch T-test, respectively, while cumulative incidence of MEs was compared between BAP1-MT and BAP1-WT using subdistribution hazard ratio (SD-HR) analysis. Analyses were performed using R package (R Foundation, v4.1).
Results: Median patient age at diagnosis was 58 years, with 20 (20.8%) patients presenting with metastatic disease at the time of diagnosis. Most patients were males (62, 64.6%), and underwent nephrectomy (84, 87.5%). Median follow-up was 52 months [IQR 22.25 – 78.25 months]. BAP1-MT and BAP1-WT did not differ significantly by age or BMI (p > 0.05). BAP1-MT patients had a higher AJCC stage on nephrectomy (p < 0.0001), with higher overall cumulative MEs (SD-HR 2.1, 95% CI 1.0-4.5, p = 0.05). Specifically, we noted a high incidence of MEs in bone (SD-HR 5.5, p = 0.02, 95% CI 1.3-23.5) followed by soft tissue (SD-HR 2.7, p = 0.001, 95% CI 1.5 – 5.0) (Figure 1).
Conclusions: Mutations of the BAP1 gene were associated with higher stage disease and incidence of metastases overall, with a higher cumulative incidence of metastases in bone compared to soft tissue compartments, suggesting a potential metastatic phenotype for this mutation.
Source of Funding: None

.jpg)
.jpg)