Back
Poster, Podium & Video Sessions
Podium
PD59: Kidney Cancer: Advanced (including Drug Therapy) II
PD59-08: International Multi-Institutional Characterization of the Perioperative Morbidity of Metastasectomy for Renal Cell Carcinoma
Monday, May 16, 2022
2:10 PM – 2:20 PM
Location: Room 255
Timothy Lyon*, Jacksonville, FL, Eduard Roussel, Leuven, Belgium, Vidit Sharma, Rochester, MN, Gianpiero Carames, Jacksonville, FL, Christine Lohse, Stephen Boorjian, Houston Thompson, Rochester, MN, Steven Joniau, Maarten Albersen, Leuven, Belgium, Bradley Leibovich, Rochester, MN

Timothy D. Lyon, MD
Mayo Clinic
Podium Presenter(s)
Introduction: Although complete surgical resection of metastatic renal cell carcinoma (mRCC) has been associated with improved cancer-specific survival, high-quality data on its perioperative morbidity are lacking. The existing population-based data are severely limited by reliance on billing claims to identify outcomes, which may overestimate events due to lack of code specificity. Therefore, the objective of this study was to evaluate 30-day complications after metastasectomy from two high-volume surgical centers.
Methods: Prospectively maintained nephrectomy registries at Mayo Clinic and UZ Leuven were queried to identify adults who underwent a metastasectomy for mRCC between 2006 and 2020. Records were retrospectively reviewed to identify a comprehensive list of over 40 possible complications within 30 days of surgery classified according to the Clavien-Dindo system, with grade III-V complications considered major. Associations of features with postoperative complications were evaluated using conditional logistic regression models with center as a stratification variable.
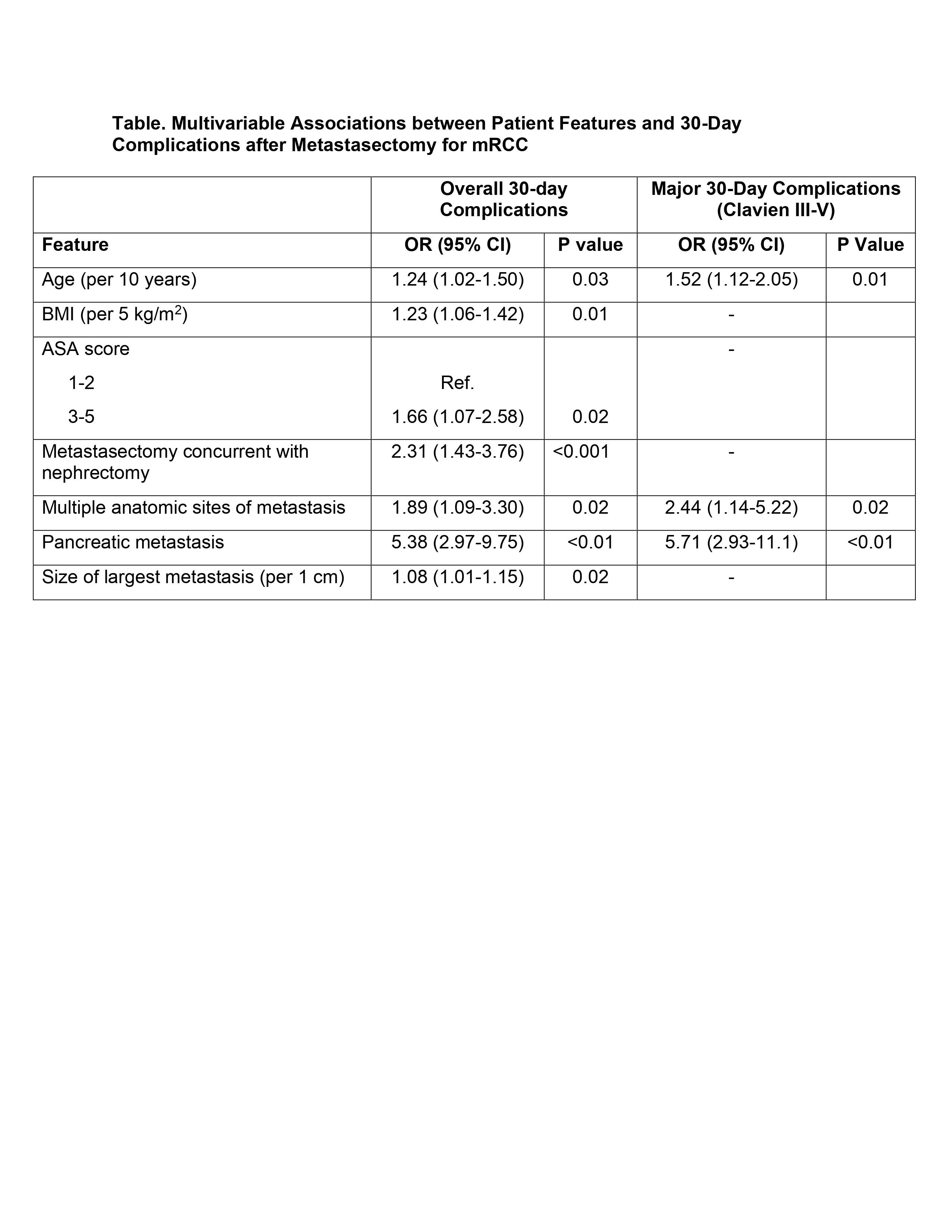
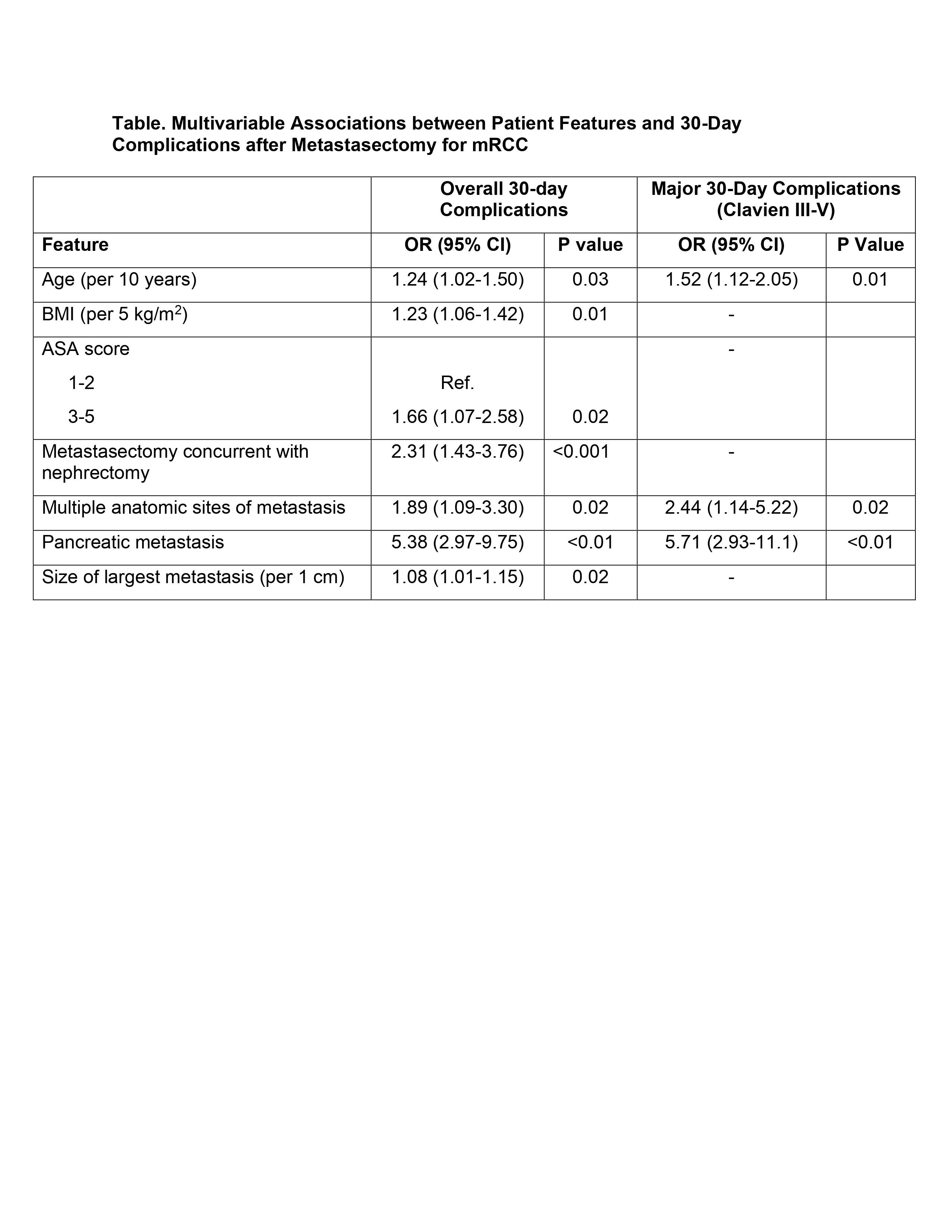
Results: A total of 740 metastasectomies in 522 patients were identified, including 543 contributed by Mayo Clinic and 197 by UZ Leuven. Among the 740 metastasectomies, 193 (26%; 95% CI 23-29%) had a 30-day complication and 62 (8%; 95% CI 7-11%) had a major complication, including eight (1%) perioperative deaths. Age, BMI, ASA score, metastasectomy concurrent with nephrectomy, multiple sites of metastasis, pancreatic metastasis, and size of metastasis were significantly associated with postoperative complications (Table). Similarly, age, multiple sites of metastasis, and pancreatic metastasis were significantly associated with major complications (Table). The addition of the indicator for complete metastasectomy and all two-way interactions with this feature was not statistically significant (p=0.2).
Conclusions: In this multi-institutional cohort fewer than 10% of metastasectomies for mRCC resulted in a major complication within 30 days, which is considerably lower than reported in population-based data. Along with increasing age and comorbidity, patients with multiple sites of disease or those who harbor pancreatic metastases are at highest risk of postoperative morbidity.
Source of Funding: None
Methods: Prospectively maintained nephrectomy registries at Mayo Clinic and UZ Leuven were queried to identify adults who underwent a metastasectomy for mRCC between 2006 and 2020. Records were retrospectively reviewed to identify a comprehensive list of over 40 possible complications within 30 days of surgery classified according to the Clavien-Dindo system, with grade III-V complications considered major. Associations of features with postoperative complications were evaluated using conditional logistic regression models with center as a stratification variable.
Results: A total of 740 metastasectomies in 522 patients were identified, including 543 contributed by Mayo Clinic and 197 by UZ Leuven. Among the 740 metastasectomies, 193 (26%; 95% CI 23-29%) had a 30-day complication and 62 (8%; 95% CI 7-11%) had a major complication, including eight (1%) perioperative deaths. Age, BMI, ASA score, metastasectomy concurrent with nephrectomy, multiple sites of metastasis, pancreatic metastasis, and size of metastasis were significantly associated with postoperative complications (Table). Similarly, age, multiple sites of metastasis, and pancreatic metastasis were significantly associated with major complications (Table). The addition of the indicator for complete metastasectomy and all two-way interactions with this feature was not statistically significant (p=0.2).
Conclusions: In this multi-institutional cohort fewer than 10% of metastasectomies for mRCC resulted in a major complication within 30 days, which is considerably lower than reported in population-based data. Along with increasing age and comorbidity, patients with multiple sites of disease or those who harbor pancreatic metastases are at highest risk of postoperative morbidity.
Source of Funding: None

.jpg)
.jpg)