Back
Poster, Podium & Video Sessions
Podium
PD59: Kidney Cancer: Advanced (including Drug Therapy) II
PD59-09: Outcomes of Cytoreductive Nephrectomy Followed by Active Surveillance in Metastatic Renal Cell Carcinoma
Monday, May 16, 2022
2:20 PM – 2:30 PM
Location: Room 255
Sari Khaleel*, New York, NY, Andrew Silagy, Melbourne, Australia, Cihan Duzgol, Ritesh Kotecha, Philip Rappold, Robert Motzer, Paul Russo, Jonathan Coleman, Martin Voss, Ari Hakimi, New York, NY
Sari S. Khaleel, MD, MSC
MSKCC
Podium Presenter(s)
Introduction: Cytoreductive nephrectomy (CRN) for management of metastatic renal cell carcinoma (mRCC) has been recently debated with the introduction of effective systemic therapy (ST) agents. However, these STs are not without significant side effects and morbidity, with current evidence supporting the continued utilization of CRN with active surveillance (CRN + AS) in properly selected patients. We retrospectively evaluated clinical outcomes of ST-naïve mRCC patients undergoing CRN followed by active surveillance (CRN+AS), subclassified into favorable- and unfavorable-risk based on prognostic criteria proposed by Rini et al (2016) for length of AS after CRN.
Methods: We searched our institutional mRCC database for ST-naïve patients undergoing CRN+AS between 1989-2020. We assessed intervention-free survival (IFS), overall survival (OS) and cancer-specific survival (CSS). Categorical and continuous outcomes were assessed using Chi-squared and Welch T-test, respectively. Cox proportional hazard regression (PHR) was used to model predictors against survival outcomes. Analyses were performed using R v4.0.4 (The R Foundation for Statistical Computing).
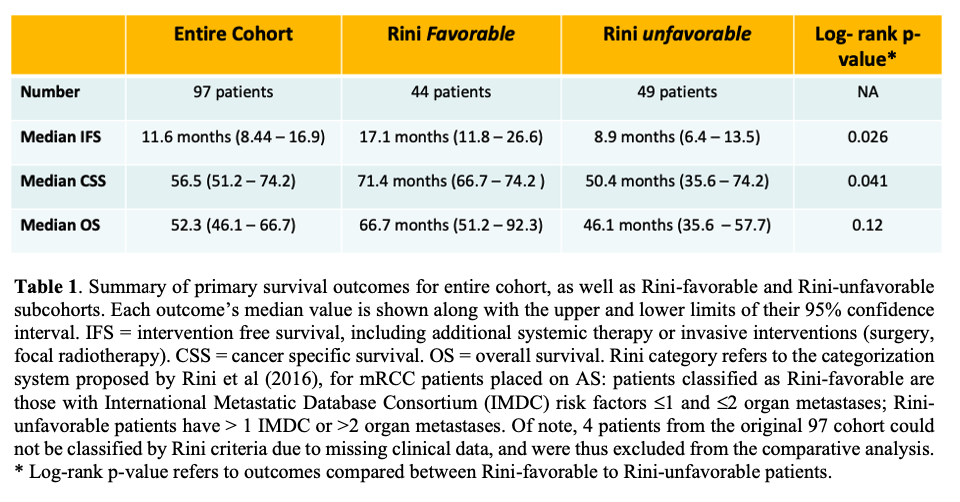
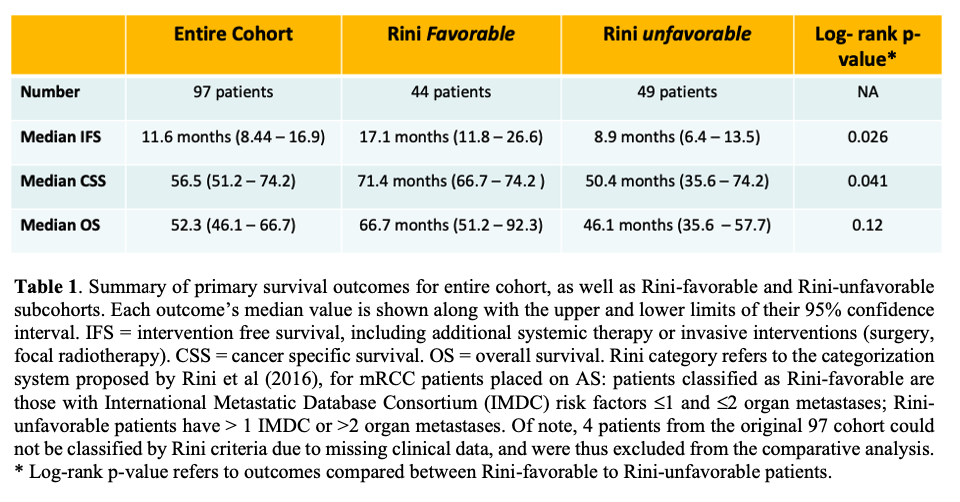
Results: Of 517 ST-naïve patients who underwent CRN, 414 (80%) had residual disease, followed by AS vs ST in 97 (23.4%) vs 295 (76.6%) patients. Patients managed with CRN+AS were older than CRN + ST patients (median age 59.7 vs 66.7 years, p < 0.001), but had no significant difference in stage or number of organ metastases. Median follow-up was 31.8 months (95% CI: 16.5 – 45.2). Median IFS was 11.6 months in the CRN+AS cohort, with 58 patients undergoing further ST/other interventions. Median OS and CSS were 52.3 and 56.5 months, respectively (Table 1). On Cox PHR, unfavorable Rini-risk was significantly associated with shorter IFS (HR 1.7; p=0.028), CSS (HR 2.1; p=0.03), but not OS (HR 1.74; p = 0.07) patients, adjusting for sarcomatoid histology and Charlson comorbidity index.
Conclusions: In this retrospective study, mRCC patients selected for primary CRN+AS had median IFS of 11.6 months, supporting CRN+AS in well-selected patients, deferring the morbidity of additional ST. Prognostic criteria proposed by Rini et al for CRN+AS patients may aid in patient selection and management planning for these patients.
Source of Funding: None
Methods: We searched our institutional mRCC database for ST-naïve patients undergoing CRN+AS between 1989-2020. We assessed intervention-free survival (IFS), overall survival (OS) and cancer-specific survival (CSS). Categorical and continuous outcomes were assessed using Chi-squared and Welch T-test, respectively. Cox proportional hazard regression (PHR) was used to model predictors against survival outcomes. Analyses were performed using R v4.0.4 (The R Foundation for Statistical Computing).
Results: Of 517 ST-naïve patients who underwent CRN, 414 (80%) had residual disease, followed by AS vs ST in 97 (23.4%) vs 295 (76.6%) patients. Patients managed with CRN+AS were older than CRN + ST patients (median age 59.7 vs 66.7 years, p < 0.001), but had no significant difference in stage or number of organ metastases. Median follow-up was 31.8 months (95% CI: 16.5 – 45.2). Median IFS was 11.6 months in the CRN+AS cohort, with 58 patients undergoing further ST/other interventions. Median OS and CSS were 52.3 and 56.5 months, respectively (Table 1). On Cox PHR, unfavorable Rini-risk was significantly associated with shorter IFS (HR 1.7; p=0.028), CSS (HR 2.1; p=0.03), but not OS (HR 1.74; p = 0.07) patients, adjusting for sarcomatoid histology and Charlson comorbidity index.
Conclusions: In this retrospective study, mRCC patients selected for primary CRN+AS had median IFS of 11.6 months, supporting CRN+AS in well-selected patients, deferring the morbidity of additional ST. Prognostic criteria proposed by Rini et al for CRN+AS patients may aid in patient selection and management planning for these patients.
Source of Funding: None

.jpg)
.jpg)