Back
Poster, Podium & Video Sessions
Podium
PD59: Kidney Cancer: Advanced (including Drug Therapy) II
PD59-10: Improving Decision-Making for Cytoreductive Nephrectomy by Evaluating Pre-Surgical Radiographic Tumor Characteristics
Monday, May 16, 2022
2:30 PM – 2:40 PM
Location: Room 255
Daniel Shapiro*, Madison, WI, Jose Karam, Alberto Pieretti, Mary Westerman, Houston, TX, Philippe Spiess, Tampa, FL, Viraj Master, Atlanta, GA, Jay Raman, Hershey, PA, Wade Sexton, Tampa, FL, Glenn Allen, Madison, WI, Surena Matin, Christopher Wood, Houston, TX, E. Jason Abel, Madison, WI
.jpg)
Daniel Shapiro, MD
University of Wisconsin School of Medicine and Public Health
Podium Presenter(s)
Introduction: Clinicians commonly evaluate different radiographic tumor characteristics as surrogates for tumor biology. Few data are available to evaluate which tumor measurements are most prognostic for survival. This study evaluated which radiographic characteristics were most likely to improve patient decision-making among patients with mRCC undergoing cytoreductive nephrectomy (CN).
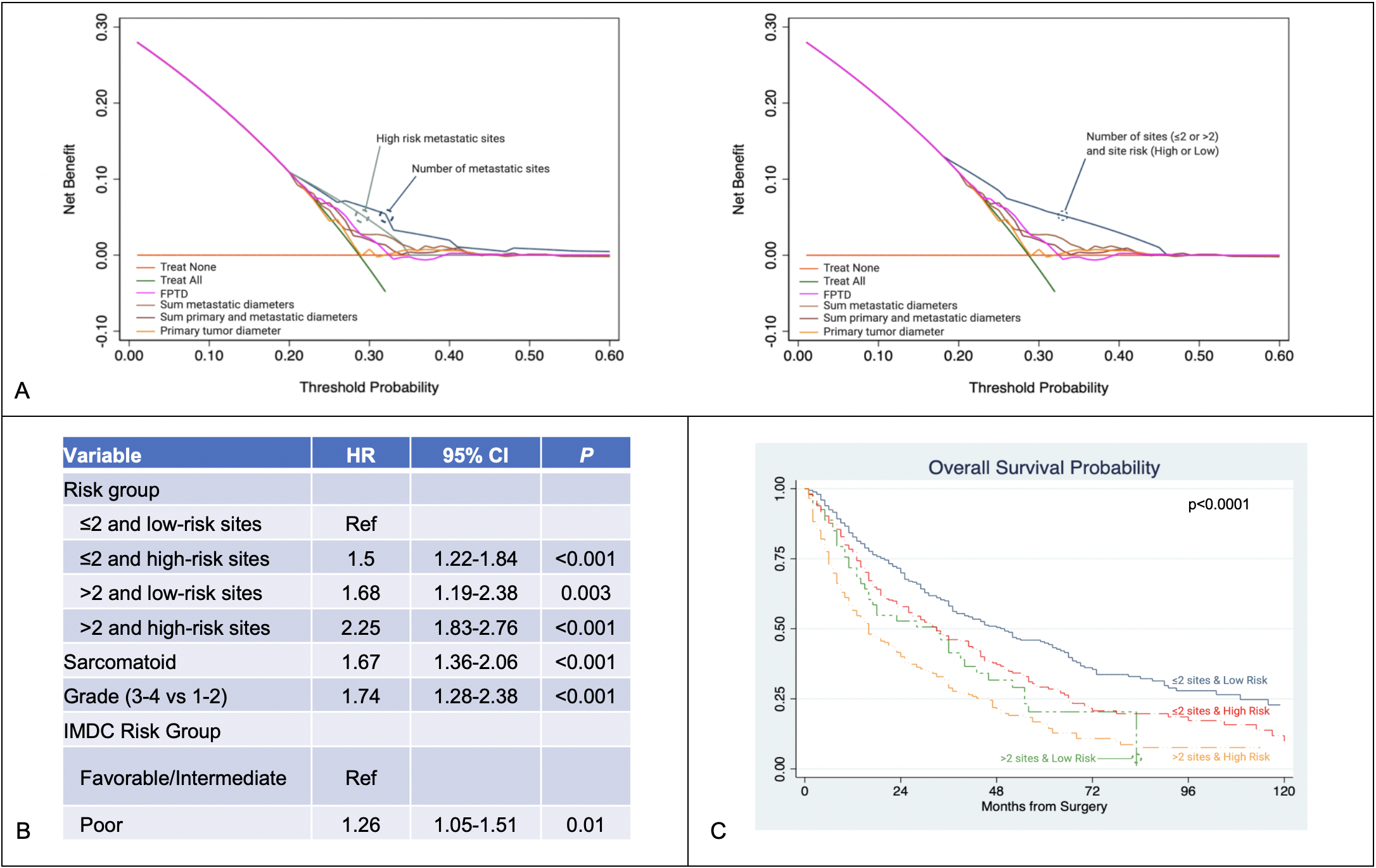
Methods: Consecutive mRCC patients from 5 centers treated with CN from 2006-2017 were included. We evaluated frequently reported tumor measurements including maximum primary tumor (PT) diameter, number/location of metastases, metastatic tumor diameters, sum of PT + metastatic tumor diameters, and fractional percent of PT diameter (FPTD) defined as PT diameter/ (total PT + metastatic tumor diameters). Cox regression determined variable association with overall survival (OS). Decision curve analysis (DCA) determined which measurements provided the most benefit when incorporated in shared decision-making after setting our outcome to death within 1 year of CN.
Results: 914 patients underwent CN with a median follow-up of 42.5 months. No difference in OS was found between upfront CN or upfront systemic therapy (n=214) when measured from date of diagnosis (p=0.6) or date of surgery (p=0.5). Univariable Cox models demonstrated that all 5 summary tumor measurements were associated with OS (p=0.01 for all). Liver, retroperitoneal lymph nodes, bowel and bone were all associated with worse OS (p=0.004 for all) when compared to other metastatic locations.
DCA demonstrated that number of metastatic sites and presence of high-risk sites provide the greatest prognostic benefit when incorporated in decision making compared to other tumor measures (Fig. 1a). A multivariable Cox model further demonstrated the prognostic value of number of metastatic sites and presence of high-risk sites to be independently associated with OS after adjusting for sarcomatoid features, IMDC risk group, and tumor grade (Fig. 1b-c).
Conclusions: Number of metastatic sites and presence of high-risk locations (liver, lymph nodes, bowel and bone) are most prognostic for survival among patients treated with CN and should be incorporated into the decision-making process for surgical intervention.
Source of Funding: None
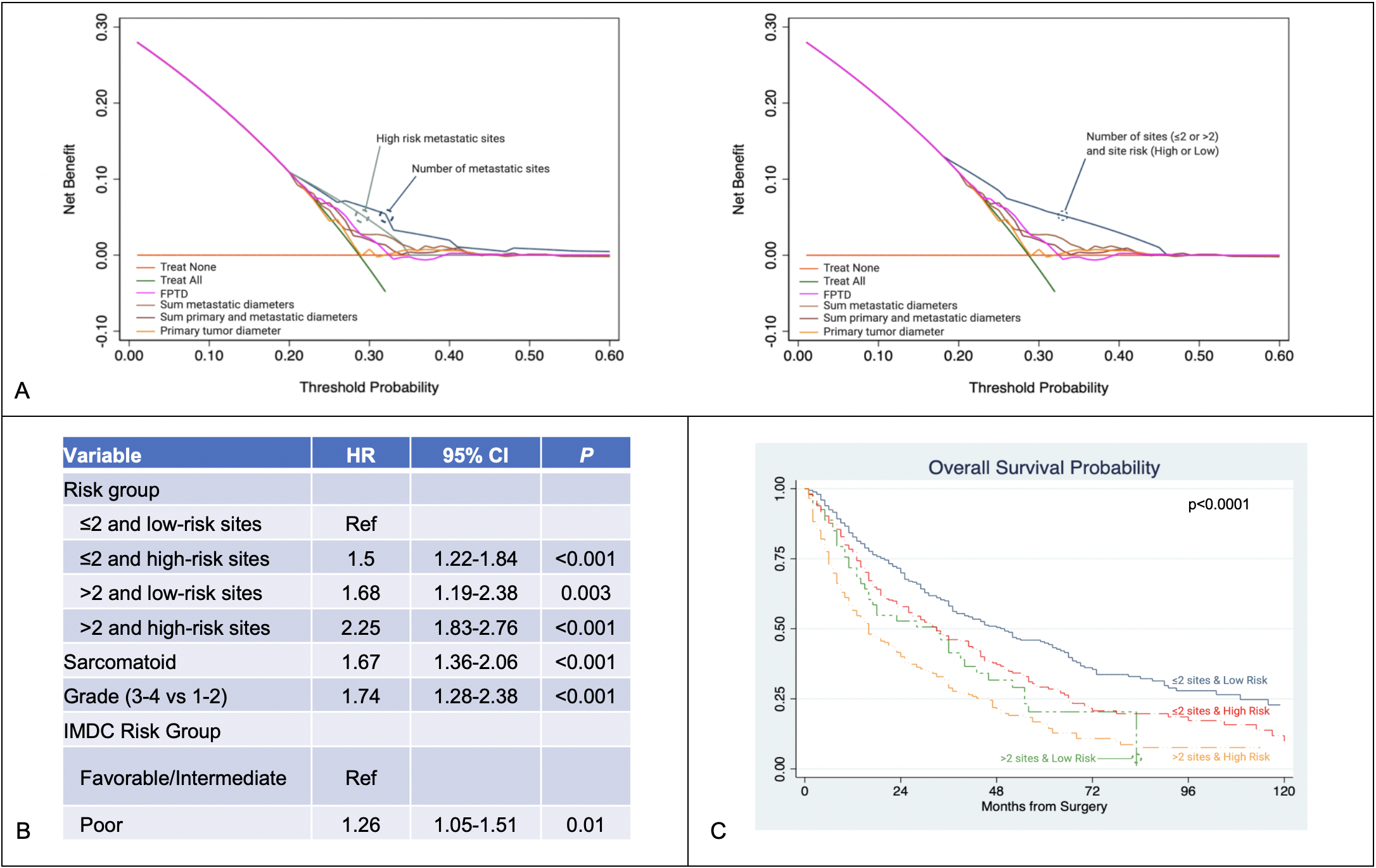
Methods: Consecutive mRCC patients from 5 centers treated with CN from 2006-2017 were included. We evaluated frequently reported tumor measurements including maximum primary tumor (PT) diameter, number/location of metastases, metastatic tumor diameters, sum of PT + metastatic tumor diameters, and fractional percent of PT diameter (FPTD) defined as PT diameter/ (total PT + metastatic tumor diameters). Cox regression determined variable association with overall survival (OS). Decision curve analysis (DCA) determined which measurements provided the most benefit when incorporated in shared decision-making after setting our outcome to death within 1 year of CN.
Results: 914 patients underwent CN with a median follow-up of 42.5 months. No difference in OS was found between upfront CN or upfront systemic therapy (n=214) when measured from date of diagnosis (p=0.6) or date of surgery (p=0.5). Univariable Cox models demonstrated that all 5 summary tumor measurements were associated with OS (p=0.01 for all). Liver, retroperitoneal lymph nodes, bowel and bone were all associated with worse OS (p=0.004 for all) when compared to other metastatic locations.
DCA demonstrated that number of metastatic sites and presence of high-risk sites provide the greatest prognostic benefit when incorporated in decision making compared to other tumor measures (Fig. 1a). A multivariable Cox model further demonstrated the prognostic value of number of metastatic sites and presence of high-risk sites to be independently associated with OS after adjusting for sarcomatoid features, IMDC risk group, and tumor grade (Fig. 1b-c).
Conclusions: Number of metastatic sites and presence of high-risk locations (liver, lymph nodes, bowel and bone) are most prognostic for survival among patients treated with CN and should be incorporated into the decision-making process for surgical intervention.
Source of Funding: None

.jpg)
.jpg)