Back
Poster, Podium & Video Sessions
Podium
PD60: Prostate Cancer: Localized: Surgical Therapy V
PD60-05: A 20 year Follow-Up Study of Oncologic Outcomes, Quality of Life and Complications in Patients Undergoing Robotic Radical Prostatectomy
Monday, May 16, 2022
1:40 PM – 1:50 PM
Location: Room 245
Alexander Bandin*, Ilene Staff, Joseph Tortora, Kevin Pinto, Tara McLaughlin, Rosa Negron, Laura OlivoValintin, Hartford, CT, Caner Dinlenc, New York, NY, Joseph Wagner, Hartford, CT
- AB
Podium Presenter(s)
Introduction: Within 10 years of its approval, surgeons were using the Da Vinci surgical robot for the majority of prostatectomies in the USA. Here we evaluate a single surgeon’s 20 year experience with robotic radical prostatectomy.
Methods: Patients were identified via an IRB approved prospectively maintained prostate cancer database. Perioperative variables such as operative time were recorded at time of surgery. EPIC 26 and/or UCLA Prostate Cancer Index scores were collected preoperatively and at each postoperative visit. PSAs, salvage and adjuvant treatment, and complications were prospectively collected. Continence was defined as 0 pads or 1 pad with occasional dribbling. Potency was defined as intercourse or an erection sufficient for intercourse within the last 4 weeks. Biochemical recurrence was defined as a PSA >0.2 or a hypersensitive PSA resulting in early salvage therapy. All surgeries were performed by a single surgeon; the initial 74 cases were performed as a co-surgeon with another fellowship trained minimally invasive urologic surgeon. Patients were divided into five year cohorts (Cohort A 2001-2005; cohort B 2006-2010; cohort C 2011-2015; Cohort D 2016-2021) and we evaluated group differences in perioperative, quality of life, and oncologic outcomes over time.
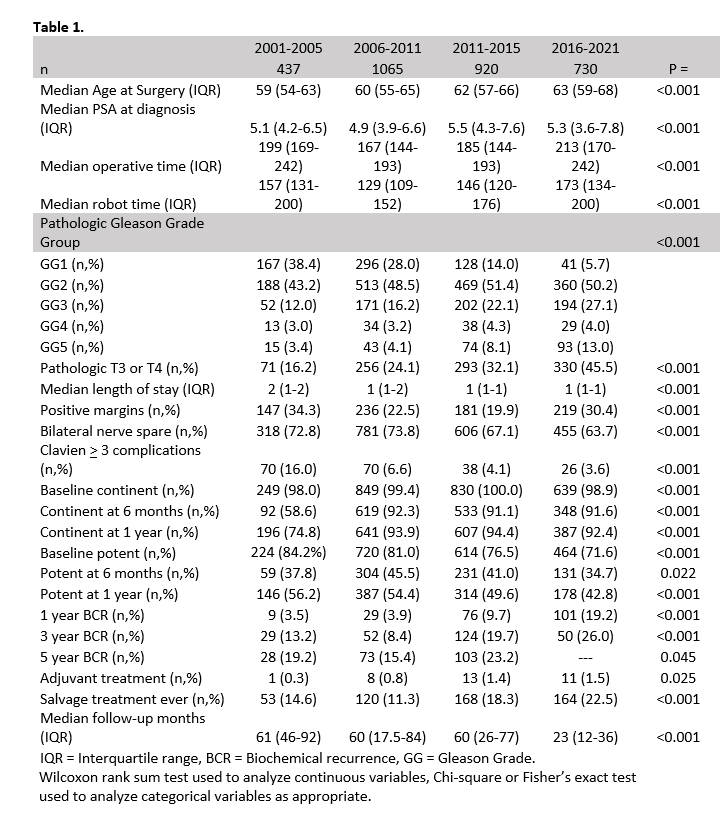
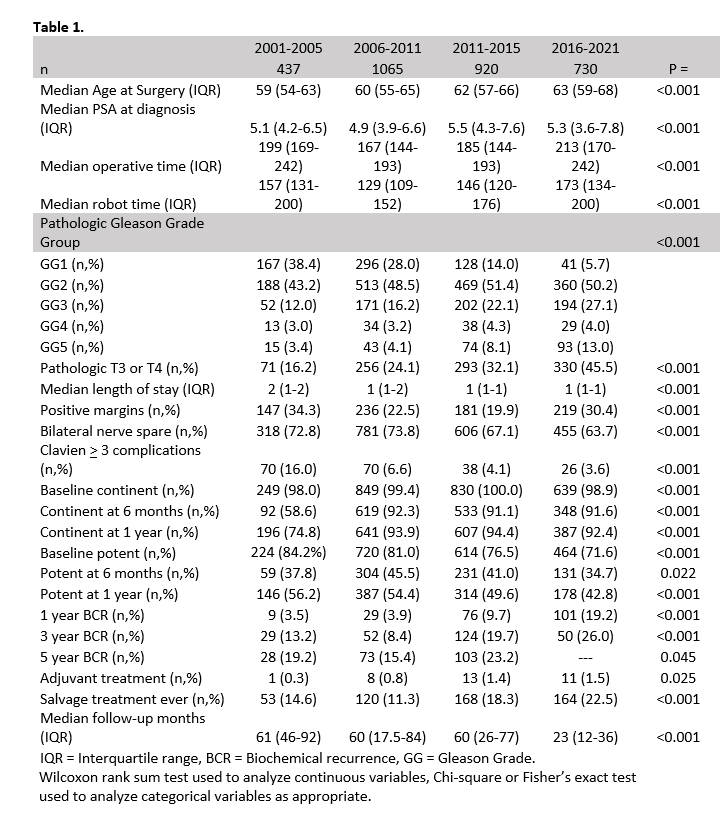
Results: 3152 patients met criteria for inclusion (Table 1). =Clavien 3 complication rates decreased from 16.0% to 3.6%, p<0.001. 1 year continence rates improved from 74.8% to greater than 92%, p<0.001. Operative times dropped from Cohort A to B (199 min v 167 min, p<0.001) and then began to gradually increase with increased resident and fellow involvement. There was considerable grade and stage migration between 2001 and 2021, p<0.001.
Conclusions: In this 20 year review of our experience with robotic prostatectomy, complication rates and continence improved over time. Confounding factors such as grade/stage migration, changes in prostate cancer screening, level of resident/fellow involvement, the advent of hypersensitive PSA, and changing recommendations for adjuvant/salvage therapy certainly influenced outcomes such as operative time, BCR, and margin status. Nonetheless, this study provides insight into the changing landscape of prostate cancer treatment over the past two decades.
Source of Funding: Unfunded
Methods: Patients were identified via an IRB approved prospectively maintained prostate cancer database. Perioperative variables such as operative time were recorded at time of surgery. EPIC 26 and/or UCLA Prostate Cancer Index scores were collected preoperatively and at each postoperative visit. PSAs, salvage and adjuvant treatment, and complications were prospectively collected. Continence was defined as 0 pads or 1 pad with occasional dribbling. Potency was defined as intercourse or an erection sufficient for intercourse within the last 4 weeks. Biochemical recurrence was defined as a PSA >0.2 or a hypersensitive PSA resulting in early salvage therapy. All surgeries were performed by a single surgeon; the initial 74 cases were performed as a co-surgeon with another fellowship trained minimally invasive urologic surgeon. Patients were divided into five year cohorts (Cohort A 2001-2005; cohort B 2006-2010; cohort C 2011-2015; Cohort D 2016-2021) and we evaluated group differences in perioperative, quality of life, and oncologic outcomes over time.
Results: 3152 patients met criteria for inclusion (Table 1). =Clavien 3 complication rates decreased from 16.0% to 3.6%, p<0.001. 1 year continence rates improved from 74.8% to greater than 92%, p<0.001. Operative times dropped from Cohort A to B (199 min v 167 min, p<0.001) and then began to gradually increase with increased resident and fellow involvement. There was considerable grade and stage migration between 2001 and 2021, p<0.001.
Conclusions: In this 20 year review of our experience with robotic prostatectomy, complication rates and continence improved over time. Confounding factors such as grade/stage migration, changes in prostate cancer screening, level of resident/fellow involvement, the advent of hypersensitive PSA, and changing recommendations for adjuvant/salvage therapy certainly influenced outcomes such as operative time, BCR, and margin status. Nonetheless, this study provides insight into the changing landscape of prostate cancer treatment over the past two decades.
Source of Funding: Unfunded

.jpg)
.jpg)