Back
Poster, Podium & Video Sessions
Podium
PD60: Prostate Cancer: Localized: Surgical Therapy V
PD60-10: A More Extended Pelvic Lymph Node Dissection Decreases Recurrence Rates in Selected Prostate Cancer Patients Undergoing Radical Prostatectomy
Monday, May 16, 2022
2:30 PM – 2:40 PM
Location: Room 245
Giorgio Gandaglia*, Giuseppe Rosiello, Milano, Italy, Francesco Pellegrino, Milan, Italy, Antony Pellegrino, Marco Bandini, Andrea Salonia, Manuela Tutolo, Mario De angelis, Milano, Italy, Gabriele Sorce, Elio Mazzone, Armando Stabile, Vito Cucchiara, Emanuele Zaffuto, Milan, Italy, Pierre I. Karakiewicz, Montreal, Canada, Shahrokh F. Shariat, Vienna, Austria, Vincenzo Mirone, Napoli, Italy, Francesco Montorsi, Alberto Briganti, Milano, Italy

Giorgio Gandaglia
Department of Urology, San Raffaele Hospital
Podium Presenter(s)
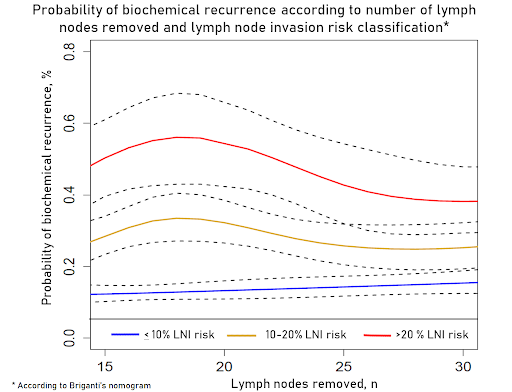
Introduction: The impact of the pelvic lymph node dissection (PLND) on the outcome of patients with prostate cancer (pCa) is still a matter of debate. We hypothesized that the extent of PLDN on the risk of developing biochemical recurrence (BCR) after robot-assisted radical prostatectomy (RARP) varies according to patient baseline characteristics and the probability of lymph node involvement (LNI).
Methods: Overall, 2,542 patients with localized PCa treated with RARP with PLDN at a tertiary referral center between 2010 and 2021 were included. All patients underwent an anatomically-defined extended PLND which included at least the obturatory, external and internal iliac stations and was extended to the common iliac and presacral regions according to each patient profile. Kaplan-Meier analyses assessed time to BCR, which was defined as two consecutive PSA values =0.2ng/ml and rising. An interaction test assessed whether the impact of the number of nodes removed on BCR-free survival varied according to the risk of LNI calculated by the Briganti nomogram.
Results: Median age was 64 years. The median risk of LNI according to the Briganti nomogram was 10%. The median number of removed lymph nodes was 15 (IQR: 7-19) and LNI rate was 10%. Overall, 314 patients experienced BCR at a median follow-up of 36 months. The 5-year BCR-free survival rate was 74%. The impact of the number of nodes removed on BCR-free survival varied according to the LNI risk (p=0.03). A more extended PLND was associated with decreased rates of BCR in men with a risk of LNI between 11-20% and, above 20 nodes, in those with a risk >20%. Conversely, the effect of PLND was virtually null in those with a lower risk of LNI.
Conclusions: The benefits associated with removing a higher number of nodes appears scarce in patients with low probability of LNI. Patients with a LNI risk >11% may benefit from more extended PLND due to decreasing probability of BCR. These patients represent the ideal candidates for prospective trials testing the role of PLND on patient outcomes.
Source of Funding: .
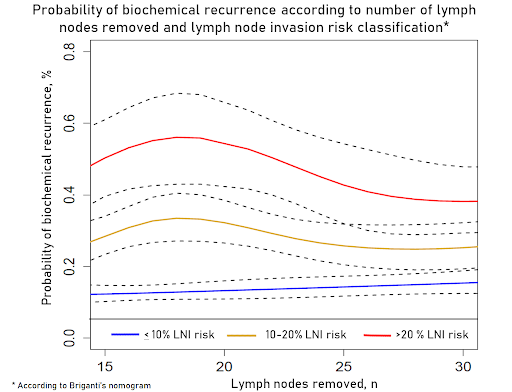
Methods: Overall, 2,542 patients with localized PCa treated with RARP with PLDN at a tertiary referral center between 2010 and 2021 were included. All patients underwent an anatomically-defined extended PLND which included at least the obturatory, external and internal iliac stations and was extended to the common iliac and presacral regions according to each patient profile. Kaplan-Meier analyses assessed time to BCR, which was defined as two consecutive PSA values =0.2ng/ml and rising. An interaction test assessed whether the impact of the number of nodes removed on BCR-free survival varied according to the risk of LNI calculated by the Briganti nomogram.
Results: Median age was 64 years. The median risk of LNI according to the Briganti nomogram was 10%. The median number of removed lymph nodes was 15 (IQR: 7-19) and LNI rate was 10%. Overall, 314 patients experienced BCR at a median follow-up of 36 months. The 5-year BCR-free survival rate was 74%. The impact of the number of nodes removed on BCR-free survival varied according to the LNI risk (p=0.03). A more extended PLND was associated with decreased rates of BCR in men with a risk of LNI between 11-20% and, above 20 nodes, in those with a risk >20%. Conversely, the effect of PLND was virtually null in those with a lower risk of LNI.
Conclusions: The benefits associated with removing a higher number of nodes appears scarce in patients with low probability of LNI. Patients with a LNI risk >11% may benefit from more extended PLND due to decreasing probability of BCR. These patients represent the ideal candidates for prospective trials testing the role of PLND on patient outcomes.
Source of Funding: .

.jpg)
.jpg)