Back
Poster, Podium & Video Sessions
Video
V05: Misc. Benign/Transplant/Renovascular
V05-12: Robotic-assisted Laparoscopic Excision of Retroperitoneal Ganglioneuroma
Saturday, May 14, 2022
2:50 PM – 3:00 PM
Location: Video Abstracts Theater
Jeffery Lin*, David Ortega, Edward Forsyth, Inderbir Gill, Los Angeles, CA
- JL
Video Presenter(s)
Introduction: Ganglioneuromas (GNs) are rare, benign tumors derived from neural crest cells. A case series of 49 GNs found tumors in the mediastinum (46%) most commonly, followed by the retroperitoneum (38.8%). Of those in the retroperitoneum, 89.5% (17/19) were in the adrenal gland. We present a case report of a para-spinal retroperitoneal GN causing right ureteral obstruction.
A 76 year old woman was incidentally found to have a retroperitoneal mass. MRI of the abdomen and pelvis showed a 6.5 right paraspinal mass with possible involvement of the L4 nerve root, causing right hydronephrosis. A right percutaneous nephroureteral stent was placed.
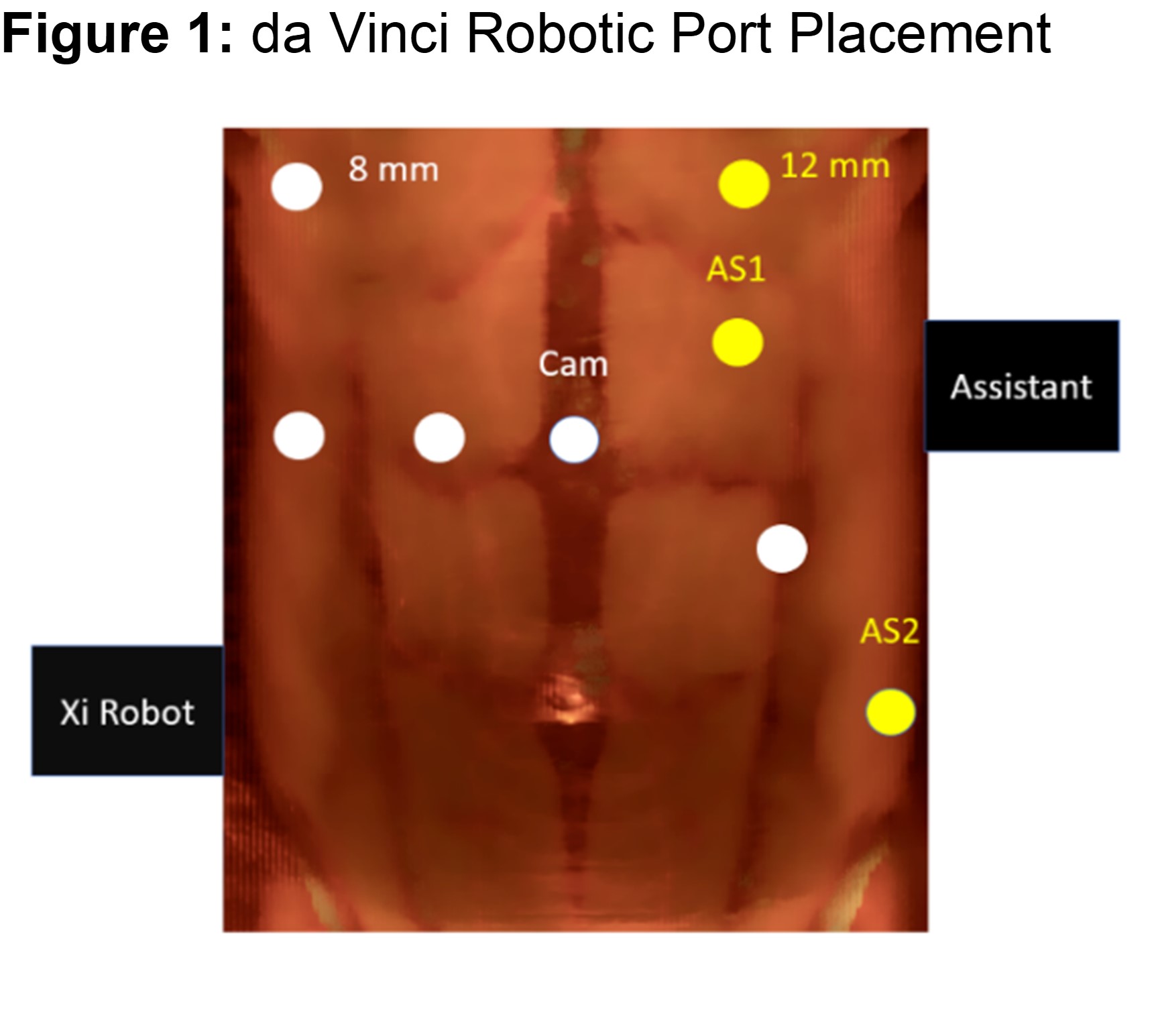
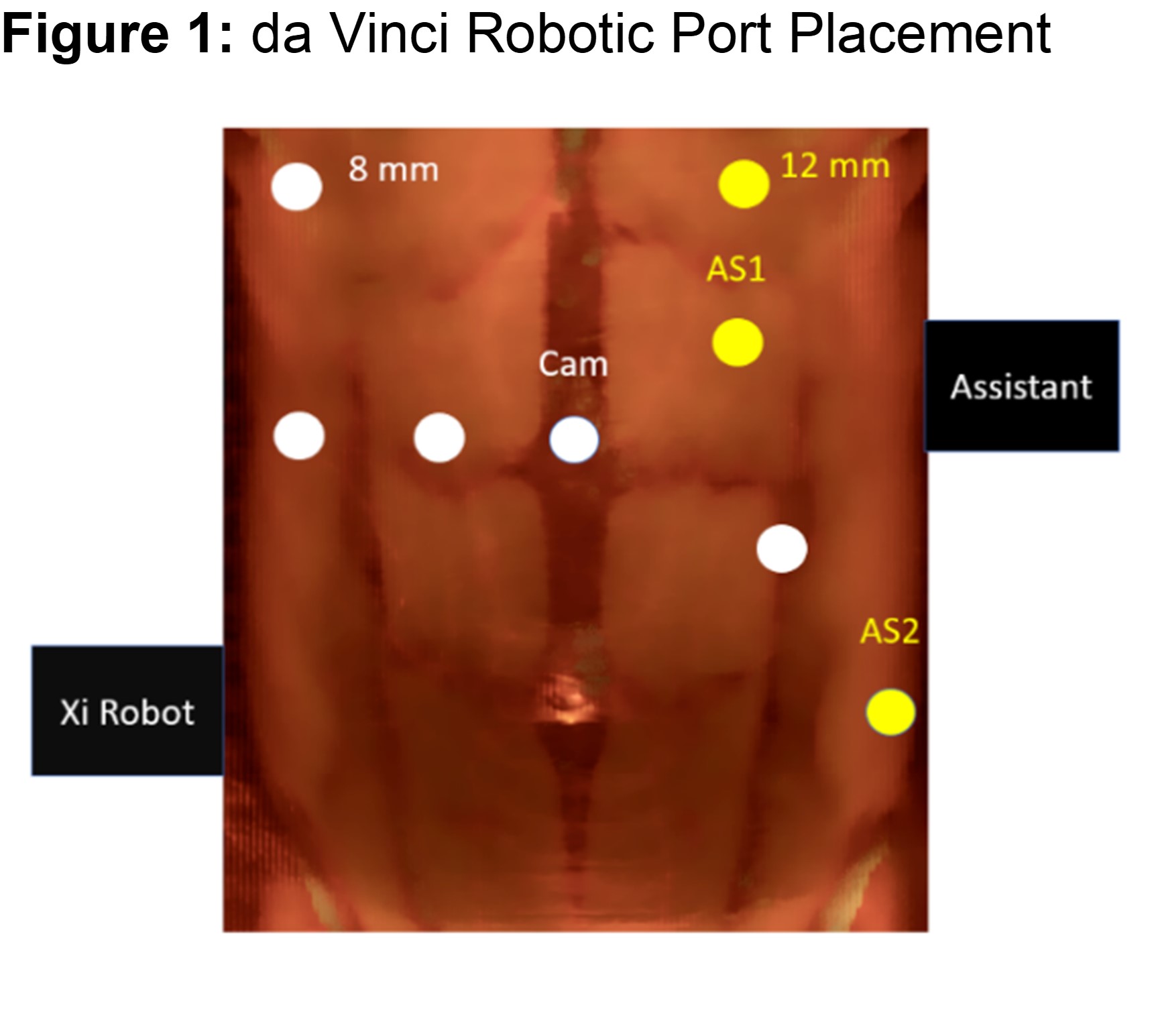
Methods: Patient was placed in dorsal lithotomy position in Trendelenberg. A da Vinci Xi robot was used (Figure 1 port placement).
After port placement, the cecum was dropped to expose the retroperitoneum. A fan retractor was utilized to retract bowel away from the surgical field. The right ureter was identified at the level of the common iliac artery and mobilized to the lower pole of the right kidney. With assistance from the neurosurgery team, the lateral border of the tumor was identified lateral to the psoas muscle. The femoral nerve was identified running anterolateral to the tumor and preserved. The tumor was separated from the right common iliac artery inferiorly and from the posterior abdominal wall posteriorly. With guidance from the neurosurgeons, the tumor was separated from the vertebral bodies medially. Care was taken to ensure preservation lumbar plexus by neuromonitoring. After the mass was excised, motor-evoked potentials pre and post-operatively showed no change.
A Blake drain was left in place with urethral catheter and nephrostomy tube to gravity.
Results: Operative time was 400 minutes with an estimated blood loss of 100 mL. The patient tolerated the procedure well and transferred to the floor. On post-operative day (POD) 2, patient was noted to have 4/5 right lower extremity strength. MRI pelvis and lumbar spine showed expected post-surgical changes with lumbar nerve roots intact. The patient was subsequently discharged home on POD3 after clearance from physical therapy and neurosurgery.
Conclusions: A minimally invasive approach is safe and feasible for peripheral nerve tumors of the retroperitoneum. With the assistance of the neurosurgical team, an excellent neurologic and urologic outcome can be achieved.
Source of Funding: None
A 76 year old woman was incidentally found to have a retroperitoneal mass. MRI of the abdomen and pelvis showed a 6.5 right paraspinal mass with possible involvement of the L4 nerve root, causing right hydronephrosis. A right percutaneous nephroureteral stent was placed.
Methods: Patient was placed in dorsal lithotomy position in Trendelenberg. A da Vinci Xi robot was used (Figure 1 port placement).
After port placement, the cecum was dropped to expose the retroperitoneum. A fan retractor was utilized to retract bowel away from the surgical field. The right ureter was identified at the level of the common iliac artery and mobilized to the lower pole of the right kidney. With assistance from the neurosurgery team, the lateral border of the tumor was identified lateral to the psoas muscle. The femoral nerve was identified running anterolateral to the tumor and preserved. The tumor was separated from the right common iliac artery inferiorly and from the posterior abdominal wall posteriorly. With guidance from the neurosurgeons, the tumor was separated from the vertebral bodies medially. Care was taken to ensure preservation lumbar plexus by neuromonitoring. After the mass was excised, motor-evoked potentials pre and post-operatively showed no change.
A Blake drain was left in place with urethral catheter and nephrostomy tube to gravity.
Results: Operative time was 400 minutes with an estimated blood loss of 100 mL. The patient tolerated the procedure well and transferred to the floor. On post-operative day (POD) 2, patient was noted to have 4/5 right lower extremity strength. MRI pelvis and lumbar spine showed expected post-surgical changes with lumbar nerve roots intact. The patient was subsequently discharged home on POD3 after clearance from physical therapy and neurosurgery.
Conclusions: A minimally invasive approach is safe and feasible for peripheral nerve tumors of the retroperitoneum. With the assistance of the neurosurgical team, an excellent neurologic and urologic outcome can be achieved.
Source of Funding: None

.jpg)
.jpg)